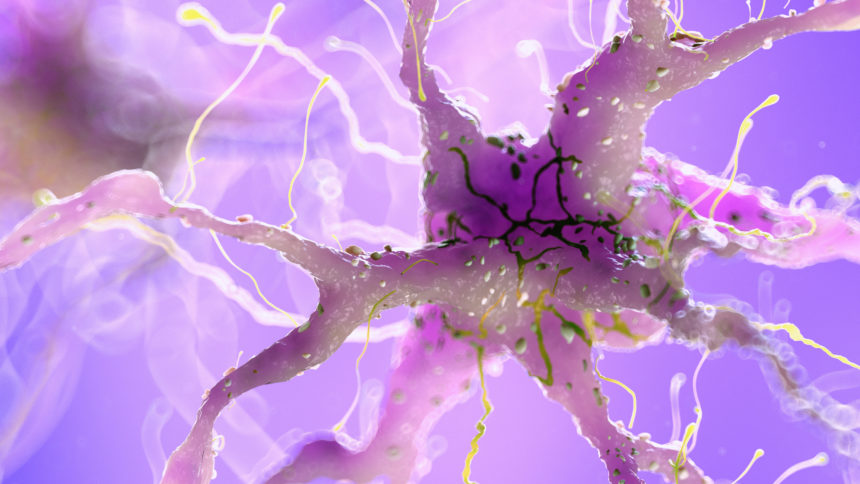
Though a lot of the talk about the cause of Alzheimer’s disease symptoms revolves around amyloid and tau proteins, a new study finds that brain inflammation is a culprit as well.
A report published Monday in JAMA Network Open points to neuroinflammation playing a prominent role in how the disease progresses. It also says there may be new pathways for developing treatments based on this discovery.
“Neuropsychiatric symptoms such as irritability, agitation, anxiety and depression are among the most difficult symptoms to treat in patients with Alzheimer’s. They are difficult to control, have no clear cause and make it difficult for families to care for their loved one without lots of support,” Cristiano Aguzzoli, MD, postdoctoral associate at University of Pittsburgh School of Medicine, and first author, said in a statement. “Here, we show for the first time that brain inflammation may be to blame for these symptoms.”
A team from the school found earlier this year that excessive brain inflammation is critical in the disease’s origins, and it can show if a cognitively unimpaired person has a higher risk for developing Alzheimer’s symptoms. The results suggested that neuroinflammation is part of the cascade that can involve amyloid beta and tau proteins and can lead to the disease.
The team’s newest results show there’s strong evidence that brain inflammation is a direct cause of neuropsychiatric symptoms that occur often in people with Alzheimer’s disease and associated dementias.
The team evaluated 109 older adults, most of whom didn’t have any cognitive impairments, but had amyloid and tau proteins present. The researchers measured levels of neuroinflammation as well as amyloid beta and tau using brain imaging. Then the scientists compared the results with clinical evaluations of neuropsychiatric symptom severity. Microglial activation was strongly linked with a variety of neuropsychiatric symptoms such as agitation and sleep interruptions, the team found. Amyloid and tau alone were predictive of neuropsychiatric symptoms, but neuroinflammation seemed to add to the symptoms, the authors said.
Neuroinflammation was most profoundly linked with caregivers or family members reporting that their loved one had rapid mood swings. In turn, participants who had caregivers with higher distress levels had higher levels of brain inflammation.
“Since both neuroinflammation and neuropsychological abnormalities are found in several other types of dementia, including Parkinson’s dementia, we are collaborating with scientists around the world to expand these findings to these other diseases,” Tharick Pascoal, MD, an associate professor of psychiatry and neurology at Pitt, also said.




