
Have you been curious as to the national data trends related to the Patient Driven Payment Model?
In a time when we are all considering changes to the future of reimbursement and the impact of potential parity adjustments, knowing your data and national trends is essential.
What is parity adjustment, you ask?
Recall that PDPM was established to be budget neutral. However, the Centers for Medicare & Medicare Services noted in its proposed rule that it’s determined, through budget neutrality analysis, that even absent COVID-related cases in 2020 (i.e., active COVID dx. and or use of the 3-day stay waiver) there was a 5.0% increase in aggregate spending under the PDPM for FY 2020 due to the shift in case mix utilization, compared to FY 2019.
How did this occur?
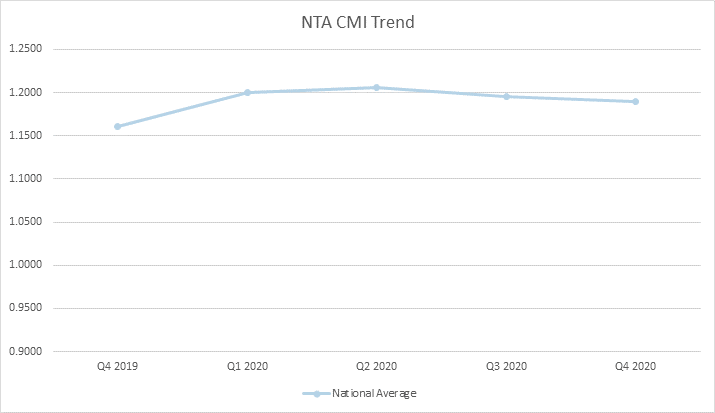
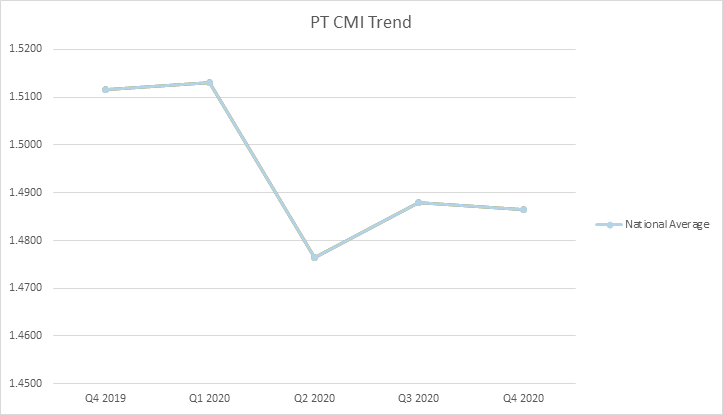
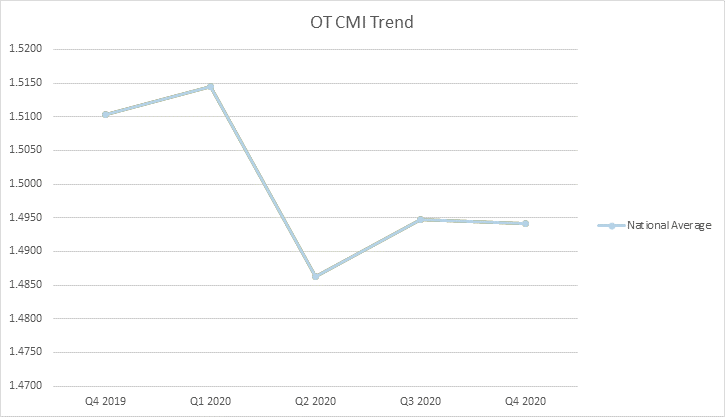
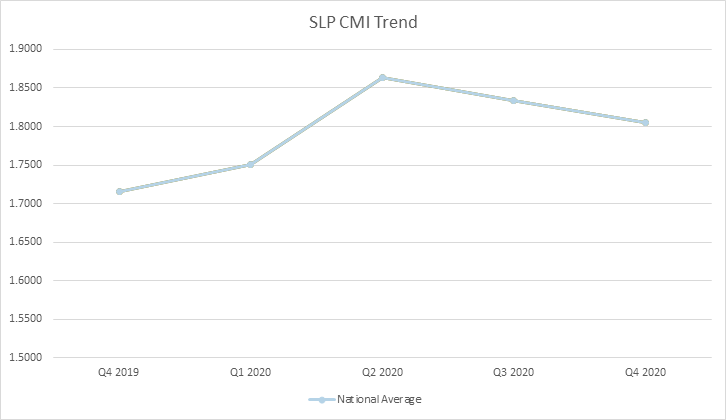
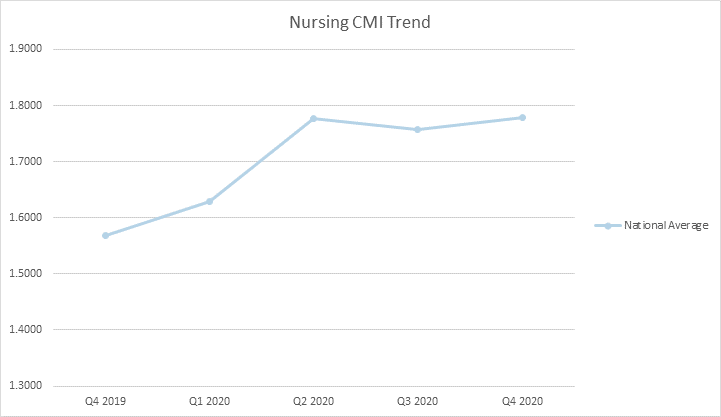
CMS observed slight decreases in the average Case Mix Index (CMI) for the Physical Therapy and Occupational Therapy rate components for skilled nursing facility populations as compared to what was expected, as well as significant increases in the average CMI for the Speech-Language Pathology (22.6%), Nursing (16.8%), and Non-Therapy Ancillary (5.6%) for FY 2020 populations as compared to what was expected for the FY 2020 SNF population.
CMS sees these significant increases in the average case-mix for these components as primarily responsible for the inadvertent increase in spending under PDPM.
Curious as to the specific trends in Q42019 thru Q42020?
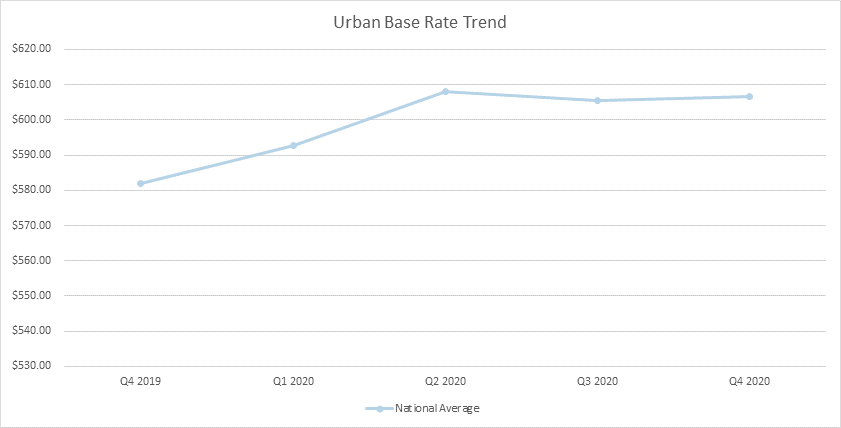
Well, you are in luck. The data is in and was recently published through CMS’ Research Data Assistance Center (ResDAC) providing insight into a full year of claims data for 2020. Below you can see overall trends from Q12019 thru Q42020 including overall rate, NTA, PT, OT, SLP, and Nursing.
What does this data and the lack of budget neutrality as outlined in Table 23 below mean for you and a potential shift to recalibration?
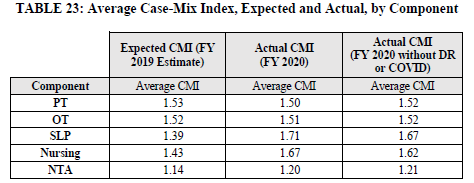
Understand that due to the indication of a 5.0% increase in spending for FY 2020 compared to FY 2019, CMS has proposed a path towards recalibration of the parity adjustment that was initially implemented with the PDPM in FY 2020 based on 2017 and 2018 data (46%), in order to achieve budget neutrality equally across all PDPM case mix adjusted components in FY 2022 (37%).
This would achieve a 5% reduction in SNF spending under PDPM, or $1.7 billion.
To accomplish this, each expected PDPM case mix index, based on 2017 and 2018 claims data, would be revised by the new parity adjustment factor of 37%. This equates to a 5% reduction in the proposed FY 2022 case mix indexes.
CMS has proposed three potential pathways to achieve parity in the PDPM rates: delayed, phased and combined delayed/phased.
Delayed
If this reduction was finalized in FY 2022 with a one-year delayed implementation, this would mean that the full 5% reduction would be prospectively applied to the PDPM CMIs in FY 2023.
If the reduction was finalized in FY 2022 with a two-year delayed implementation, then the reduction in the PDPM CMIs would be applied prospectively beginning in FY 2024.
Phased
With regard to a phased implementation strategy, this would mean that the amount of the reduction would be spread out over some number of years. Such an approach helps to mitigate the impact of the reduction in payments by applying only a portion of the reduction in a given year.
For example, if CMS were to use a two-year phased implementation approach to the 5% reduction discussed above, this would mean that the PDPM CMIs would be reduced by 2.5% in the first year of implementation and then reduced by the remaining 2.5% in the second and final year of implementation.
So, for example, if this adjustment was finalized for FY 2022, then the PDPM CMIs would be reduced by 2.5% in FY 2022 and then reduced by an additional 2.5% in FY 2023.
CMS notes that the number of years for a phased implementation approach could be as little as two years but as long as necessary to appropriately mitigate the yearly impact of the reduction.
For example, CMS could implement a five-year phased approach for this reduction, which would apply a 1% reduction to the PDPM CMIs each year for five years.
Combination Delayed/Phased
CMS also notes that mitigation strategies may be used in combination with each other.
For example, CMS could finalize a two-year phased approach with a one-year delayed implementation.
Using FY 2022 as the hypothetical year in which such an approach could be finalized, this would mean that there would be no reduction to the PDPM CMIs in FY 2022, a 2.5% reduction to the PDPM CMIs in FY 2023 and then a 2.5% reduction in the PDPM CMIs in FY 2024.
What approach will CMS take? The path is yet to be determined. For now, we can review and understand our data, compare ourselves to national trends, document to support the care we provide and prepare for the changes which undoubtedly are ahead of us all.
Renee Kinder, MS, CCC-SLP, RAC-CT, is Executive Vice President of Clinical Services for Broad River Rehab and a 2019 APEX Award of Excellence winner in the Writing–Regular Departments & Columns category. Additionally, she serves as Gerontology Professional Development Manager for the American Speech Language Hearing Association’s (ASHA) gerontology special interest group, is a member of the University of Kentucky College of Medicine community faculty and is an advisor to the American Medical Association’s Relative Value Update Committee (RUC) Health Care Professionals Advisory Committee (HCPAC).





