
The staffing crisis in long-term care is showing signs of easing, but many building leaders still want higher pay and more flexibility in exchange for the extra work they’re putting in, according to results from the 5th annual
McKnight’s Mood of the Market survey.
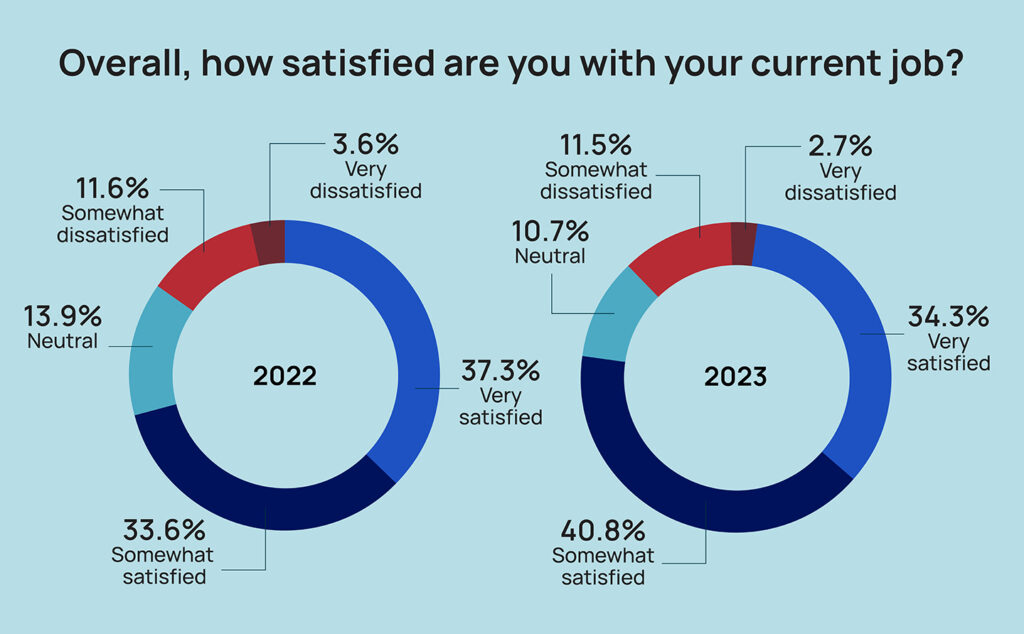
While employees last year clamored for more co-workers to improve their job satisfaction, the most desired change this year was a higher salary, with more than half of survey takers choosing that option. And despite three-quarters (75.1%) reporting being “somewhat satisfied” or “very satisfied” with their current jobs, almost one-quarter (22.6%) said they were “not so well paid,” or “not at all well paid.”
The 2023 survey drew more than 500 responses from directors of nursing and their assistants, and administrators and their assistants. They sent mixed signals about the meaningfulness of their work, their willingness to remain on the job and the changes today’s employers need to adopt to keep them.
Overall, the share of workers “very satisfied” or “somewhat satisfied” with their current job rose about 3% from the 71.9% mark of a year ago.
Cara Silletto, president and chief retention officer of Magnet Culture, said she’s hearing from clients that some staffing stability has been gained over the last six months. But she cautions that any relief from the workforce shortage shouldn’t be viewed as a return to pre-COVID normalcy. In fact, she believes many nursing home leaders see themselves with a new baseline for staffing — one that is leading them to demand better pay even after years of solid increases.
“On this particular question saying more staff will solve my problem, they’re now rolling their eyes and saying, ‘Yeah, yeah, that’d be nice,’” Silletto told McKnight’s Long-Term Care News after reviewing results. “That shrinking staff is why I think they just want higher salaries because they’re going, ‘We’re gonna have to deal with this churn. And so I just need more money because I am never fully staffed. I am never going to get caught up. I am never gonna be not trying to fill tonight’s shift.”
Staffing a ‘smidge’ better
Katie Piperata, a workforce engineer with 15 years’ experience recruiting for skilled nursing, counters that the boost in satisfaction rates and some of the other positive findings from this year’s survey are reflective of the labor crisis “getting a smidge better.”
She noted the negative “trickle-up” effect of a DON being routinely called to the floor to cover for missing nurses or aides. Administrators then have to step in on some of the DON’s duties, a reality that has hurt satisfaction among both categories of workers in the COVID era.
At National Healthcare Associates, which operates 33 facilities in the Northeast, leaders are trying to combat inflationary pressures with fair salary increases and a culture that prioritizes retention. They’ve seen increased demands for raises and higher asks from new candidates, says Anthony Scarpino, the company’s vice president of talent acquisition.
“It’s a factor of the rapid inflationary growth of salaries,” he told McKnight’s. “Your salary may fall behind in a single year.”
That could be one explanation for the 52.2% of respondents who said a higher salary would most improve their job satisfaction. That broke down to 51.3% among DONs and 52.8% among administrators.
Just 17.5% of survey respondents said they were “very well paid,” a finding that remained static year-over-year, despite recent raises that exceeded historic averages nationally. Nursing home administrator salaries averaged $127,763, up 3.6% from $123,324 in 2022. Directors of nursing saw their average pay climb 4.67% from $103,954 in 2022 to $108,889 this year, according to the annual HCS Nursing Home Salary & Benefits Report.
Every strategy ‘known to man’
As of this writing, National Healthcare Associates had no openings in its DON or assistant DON ranks, but the perception that wages are stagnant makes it that much tougher to hire when there is a vacancy, Scarpino added. Strategies to retain rather than replace get high priority at NHA.
“I can tell you that we have thought of every bonus incentive, either motivational or retention activity, that is known to man,” Scarpino said. “I think the only time that I’ve seen it more competitive is not necessarily during [the first wave of] COVID, but right after, as we were all trying to open at the same time, we were all trying to return to business.”
Although many providers are focused on competing for staff with agencies, travel nurse firms and other local healthcare entities, Silletto says there is a new foe they may not even take into consideration. That’s a massive increase in healthcare pay transparency, thanks to social media, publicly available surveys and websites, and even new legal requirements for job postings in some states.
“People talk more today about how much money they make than ever before,” she said, also quoting the adage that says, “Comparison is the thief of joy.”
Crazy comparisons
Comparisons between DONs and admins may be driving one significant split identified in the McKnight’s survey: Nearly 23% of DONs said they were “not so well paid” or “not at all well paid,” compared to 14% of administrators.
“It never surprises me that a second-in-command is less thrilled with their pay than the top paid person at any organization,” Silletto added. “A lot of people just think, ‘I should be paid just as much as the next person,’ if they see themselves in a more collaborative role.
“I honestly think there is nothing companies can do — outside of actually paying more — that can overcome this frustration people find,” she said. “When they learn how much money other people make, it is human nature to feel frustrated or jealous or angry.”
Another key finding, however, shows the disconnect between pay satisfaction and meaningful work. For the second year in a row, about 73% of respondents said they found their work “very meaningful.” Among administrators, that share inched up to 75.8%, while 68.7% of DONs reported their work was “very meaningful.”
Workers aren’t bending on flexibility
More nursing home employees also are insisting on flexible scheduling, following years of COVID conditions that have often called on them to work back-to-back shifts and take on overtime they didn’t necessarily want. Survey respondents indicated that not being able to offer flexible work is a major hiring and retention issue in a new economy shaped by the rise of the gig worker.
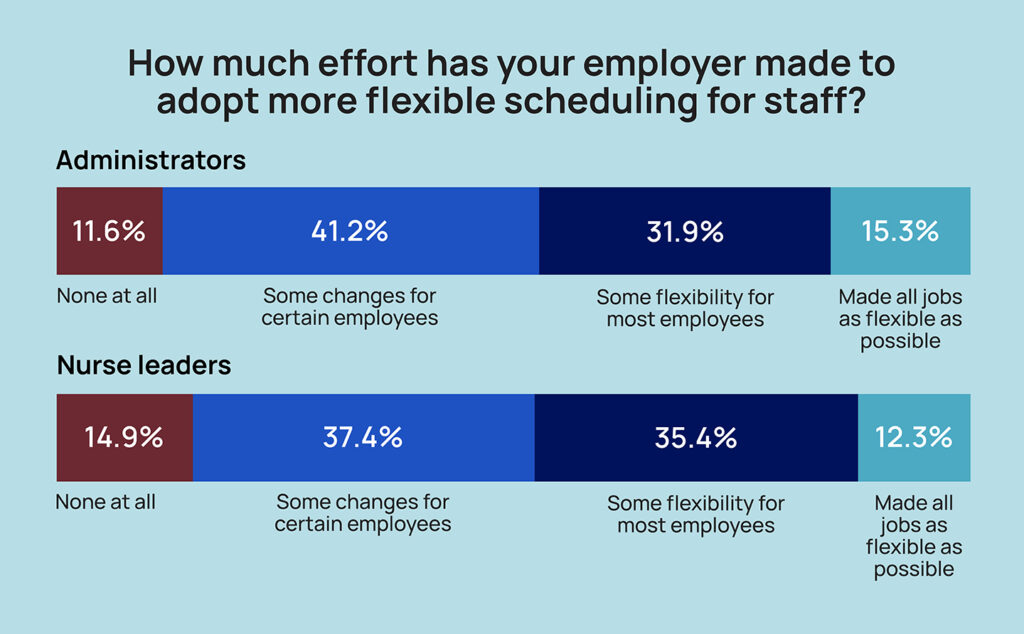
Overall, 40% of respondents told McKnight’s their workplace had made “some changes, but only for certain employees.” Another 35% said “some flexibility is now available for most employees.” That represents three-fourths (75%) of respondents, but some 13% said their facility or chain had made no effort “at all” to adopt more flexible scheduling.
“While accommodating flexible schedules can sometimes be a challenge for centers, providers need to change the way they have always done things,” said Kendra Nicastro, director of business development for healthcare recruitment firm LeaderStat. “If you are not adapting and developing new ways to attract candidates (flexible schedules, same or next-day pay options, etc.), you will continue to fall behind and recruitment and retention will continue to be a challenge.”
This was the first year that McKnight’s specifically asked whether employers were offering flexible scheduling. But in a separate question about potential changes that would most improve their job satisfaction, slightly more employees chose the option of a more flexible schedule in 2023 than in 2022, rising to 13.7% from 11.4%. Administrators were more likely than nurse leaders to choose that option at 14.6% vs. 12.3%.
Those numbers are likely far lower than if the survey had been offered to all nursing home staff, Silletto said.
“DONs and administrators have the most flexibility in the whole building. They can come and go whenever they want and if their kindergartner kid or grandkid has a two o’clock play, they can leave the building when most of their staff cannot,” she said.
Creativity emerges
That said, building operations are directly impacted by approaches that try to meet the desire for flexibility among other workers. Just under a quarter (24%) of survey respondents said their facility offered self-scheduling tools for employees; 46% had increased part-time opportunities, and 29% offered three- and four-day workweeks.
More than one-third of respondents (161) also entered an answer in “other” options that showed, for the most part, a willingness to explore flexibility. Those included the use of 12-hour shifts; PRN schedules or internal float pool; staggered shifts to accommodate school start times and other personal needs; and shift sharing.
Several respondents also noted in terse terms that their owner or corporate leadership refused to be more flexible with scheduling, or that union contracts prevented facilities from offering some options their peers had found success with.
“Most companies, honestly, haven’t had the bandwidth to explore more flexibility options,” Silletto said. “The way they’ve always scheduled, they know it’s not working, and yet, they don’t know what else to do.”
Middle ground elusive
Piperata said the leadership candidates she works with are “very much” demanding some flexibility, even if it’s just one day a week at home to catch up on all reports, emails and other non-clinical requirements. But she doesn’t see her clients, meaning nursing home HR leaders, budging much.
“When you’re leading the whole building either on the clinical or ops side, it’s the customer who wants to see you, it’s the customer who is wanting that visibility and that representation. So I get where the client is coming from on that,” said Piperata. “But I also get that we’re in this gig worker mentality. People want the flexibility to be able to have a day to get everything done or to work for longer days because staff nurses are able to do Baylor [12-hour weekend] shifts and things that do allow flexibility. So I think we’re just seeing the DON and administrator saying, ‘I want that, too.’ ”
Ted LeNeave, CEO and founder of Accura Healthcare, operates 34 skilled nursing facilities in the Midwest. While he’s hearing more requests for flexible and remote work options, he sees some positions for which that’s just not aligned with the business of doing healthcare. For instance, he recently determined a DON asking to work four days a week in the building wasn’t a “good culture fit.”
“It’s not that kind of job,” he said. “We can have flexibility in other areas, but we can’t have flexibility to not be in the facility if your job is in the facility taking care of those people.”
Scarpino takes a different view. He sees trying to be more amenable to employee desires as a way to avoid costly attrition.
“We don’t see as many people leaving the industry as we see people changing roles for additional pay, a better shift, more flexibility, a better commute,” he said. “I think the whole industry, not just senior living but healthcare in general, is really struggling with this idea of flexibility, particularly with so much attention being given to work from home outside of the industry.”
He’s exploring adding self-scheduling technology, seeing that as one of the best possible solutions. In the meantime, he’s trying to manage candidates — from leaders to brand new CNAs — who ask for special arrangements.
“We just try to be flexible with them as far as we can within the confounds of our operation,” he said. “Whether it’s a 16-hour shift, no weekends, only weekends, days, nights, evenings, those different things. There’s all kinds of different scenarios that we try to piece together to accommodate.”
Seeking solutions
Silletto applauds such flexibility and is encouraging hiring managers to think of their staff more as members of separate pods. One might be PRN and one might be part-timers; and another could be full-time, traditional eight-hour shift workers who never ask for accommodations. The employer can then pay incentives to each pod to ensure round-the-clock coverage.
“I would say an overarching theme — and employers hate to hear this, but it is a current problem — is fewer people in the workforce want to be told where to be when,” she said. “Offering as much flexibility and as many shift options and start and end times as possible helps it fit into their lives. A lot of people are less tolerant today of sacrificing for work.”
For leaders resistant to demands for flexibility, Piperata suggests testing it first in buildings where there might be less risk.
“If you have a 5-star building that’s performing well and the administrator and DON have been there a while, there hasn’t been a lot of turnover, why not allow something like that?” she asked. “I think that maybe they could start to look at it more from a custom standpoint. If your building is doing well, then you can earn this. If these two or three things are met, then this is something that we would work with you on versus just saying, across the board, ‘We’re not doing that.’
Without more change, recruiting nurses who can find the hours they want in hospitals and keeping entry-level employees who have plenty of options in retail or hospitality will continue to be a slog, Piperata said.
Reluctant providers need to think about how their stance positions them in what will only become a more competitive landscape in the coming years, Nicastro added.
“When candidates see flexible scheduling in a job description,” she said, “they can assume that your building is proactively addressing employee requests for work/life balance and working to stem burnout.”
From the October 2023 Issue of McKnight's Long-Term Care News




