
The Centers for Medicare & Medicaid Services must consider the COVID-19 pandemic’s broad impact on the skilled nursing patient population and the resulting effect it had on Medicare payments for SNF care before toying with PDPM rates, asserts a new Avalere Health analysis.
The report, issued Monday, evaluated the comprehensive impact the coronavirus pandemic had on patients by using the federal data to analyze how changes to patient care and operations may have affected Medicare payments for SNF care for both COVID and non-COVID residents.
It comes in response to federal officials’ recent proposal to adjust the parity rates after skilled nursing facilities collected $1.7 billion, or 5%, more than expected in Medicare payments in the first year of the Patient Driven Payment Model. The model was intended to be budget neutral, but it launched just months before the pandemic began and healthcare costs skyrocketed.
The study found that there was a higher proportion of SNF residents diagnosed with respiratory illnesses throughout fiscal year 2020 when compared to 2019 and 2018. The analysis also noted that guidance from CMS on COVID-19 diagnosis coding wasn’t available to SNFs until March 2020, but data shows that respiratory diagnoses were “significantly higher in all of FY 2020” compared to prior years.
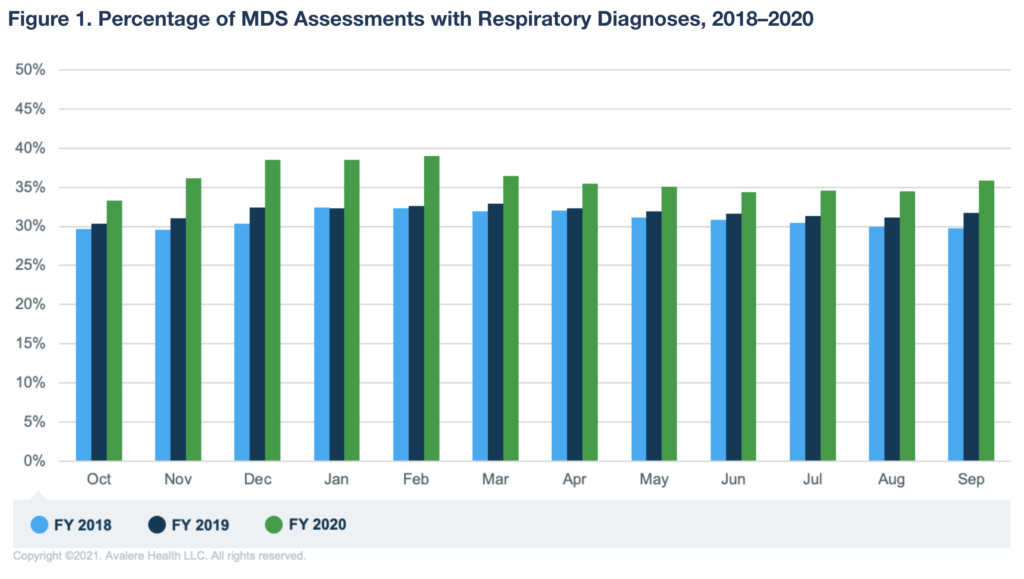
“While several factors may contribute to the higher rates of respiratory illness, it is conceivable that this sharp increase was driven in part by COVID-19 cases before the CMS instituted a formal COVID-19 diagnosis code and by undiagnosed cases throughout the year,” Avalere Health authors Fred Bentley, Melissa Morley, Emily Gillen and Heather Flynn wrote. “This finding suggests that the CMS’s claims-based approach using the COVID-19 diagnosis code may not have adequately captured the COVID-19 case volumes over the course of the pandemic.”
The analysts also looked at acuity changes of beneficiaries treated in SNFs over the course of the pandemic by investigating changes in the case-mix indices across the five components of SNF care for both COVID and non-COVID residents.
“While there were was no change in the CMI for OT, PT, or NTA, the findings indicate that the speech-language pathology and nursing CMIs increased in April 2020 for COVID-19 and non-COVID-19 patients, and the CMIs remained high for the rest of FY 2020 relative to the pre-pandemic period,” the authors explained.

They added the increase in CMI for non-COVID residents suggests the pandemic’s effects extended to the broader SNF population and not just those with a COVID-19 diagnosis.
“Our results indicate that it is hard to disentangle the impacts of the transition to the new payment system and the impacts of the COVID-19 pandemic,” Morley told McKnight’s Long-Term Care News on Tuesday.
She stressed the importance “to consider the impact of the pandemic on the non-COVID patient population as CMS evaluates the transition to PDPM.”





