
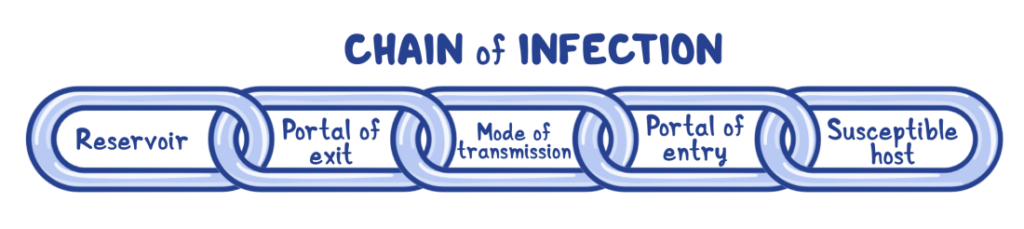
One of the basic concepts in infectious disease epidemiology is the “chain of infection” – in order for any organism to persist in the environment and cause infections, all links of the chain must be present. Infection preventionists are constantly searching for ways to break this chain and prevent infection.
Any breach in the skin presents an opportunity for microbes to live and persist, providing a potential portal of exit for these potential pathogens to escape into the environment, or providing a potential portal of entry that may lead to an infection in a susceptible host (the resident).
Breaches in the skin can certainly include medical devices, such as urinary catheters or any number of intravascular lines, but often, they are wounds. Managing wound care from an infection prevention perspective ensures that you are doing all you can to keep residents safe and free from infection.
As part of a wound care program, a facility should have policies and procedures available that specifically make clear what the expectations are regarding skin assessment and wound management – these should provide step-by-step instructions, as well as the expected frequency. The facility should train all staff on wound care both on hire and annually. Audits should be done on a regular basis using a standardized tool.
As a result of these audits, healthcare professionals providing wound care should receive the results of the audit as well as education on any gaps identified. A great standardized audit tool resource is the wound care observation checklist from the Centers for Disease Control and Prevention.
Personal protective equipment (PPE)
PPE is essential to prevent the spread of infection in facilities. The Minnesota Department of Health offers some excellent guidance for PPE during wound care. PPE should be available in all sizes, and gloves should be worn for all stages of wound care – and changed anytime one is moving from dirty to clean surfaces or supplies (this includes skin surfaces).
As always, hand hygiene should be performed between doffing old gloves and donning new gloves. If there is any chance of splashes or spray, a mask and eye protection are advised. A clean gown should be worn if arms or clothing may come into contact with a resident. Doffing PPE should be done in the correct order and placed in an appropriate receptacle.
Wound care equipment/supplies
Wound care equipment and supplies are often reusable, and any that come into contact with non-intact skin, mucous membranes or body fluids – including those on linen or the hands of a healthcare worker – should be considered semi-critical instruments and disinfected as such. This includes such common items as scissors, flashlights and rulers. For some of these items, high-level disinfection or sterilization may not be possible – in those cases, it’s best to have dedicated equipment for each resident. Always clean and disinfect equipment to reduce contamination per the manufacturer’s instructions for use (IFUs), even if that equipment is dedicated to one resident.
Dedicate tape rolls, sprays, creams and any other wound care products to one resident – do not use these items for multiple residents. Do not store used sprays or creams with clean wound care supplies. Wound care dressings should be disposed of according to facility policy, and dripping or saturated dressings should always be disposed of with biohazardous waste.
It is also important to clean and disinfect surfaces where clean wound care supplies will be placed or stored. It might not be the first thing to come to mind, but organisms on the surface can transfer to supplies, healthcare workers’ hands, and, ultimately, a resident’s wound.
Our customers constantly reinforce the importance of a simple disinfecting process for surfaces at the point of care. No matter what product you choose to disinfect surfaces at the point of care, make sure the product is an EPA-registered disinfectant designed for healthcare.
Jenny Bender, MPH, BSN, RN, CIC, and Clinical Science Liaison, PDI Northeast Region, has more than 10 years’ experience as an infection preventionist in community hospital, ambulatory/outpatient, academic medical center, behavioral health, and public health settings.
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.




