
There’s no denying that skilled nursing facilities care for unique populations. In fact, many are de facto specialty care centers with a disproportionately large number of certain types of residents. This scenario is well known within the provider community and, unfortunately, can translate into a liability in the survey/certification process and further complicate key Centers for Medicare & Medicaid Services initiatives that influence your public profile.
One example of this was brought to me by a provider specializing in the care of people with mental illness. Despite being mission focused on meeting the needs of this challenging population and supporting a significant community need, the provider felt penalized by not only the survey process and CMS’s Five-Star, but also excluded from alternative payment models and preferred networks.
Is this experience universal among SNFs specializing in the care of MI populations?
In a recently study, we examined the correlation between caring for people and negative survey, Quality Measures, and Five-Star results. We also tested if higher concentrations of mental illness (MI) were related to a longer average length of stay and higher rehospitalization.
First, we identified SNFs in the top (n= 3949) and bottom (n = 3995) quartiles of caring for people with MI; they had rates of MI at 57% and 8%, respectively. We examined outcomes across many domains to broadly address whether high concentrations of this specialty population had a negative correlation to key business drivers in the post-acute world. Results are summarized in this chart:
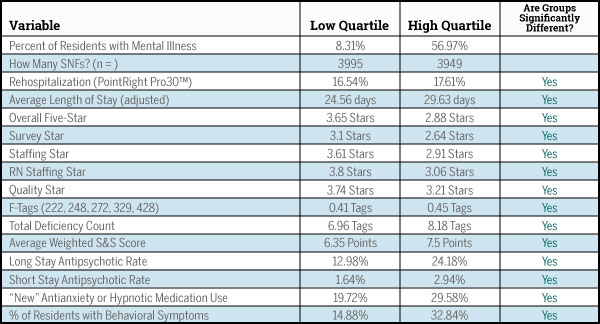
The hypotheses we tested were true: SNFs specializing in the care of people with MI had worse outcomes as measured by Five-Star (all domains), rehospitalization rates and longer lengths of stay. Although the study requires additional academic rigor to move beyond correlation to causation, all indicators point in the same direction to validate the provider’s instincts.
What to do with this information? On a societal level, we must recommit ourselves to the proper care of people with MI. As an industry, we need to embrace the reality that not all SNFs care for what might be considered “traditional” residents.
In fact, as healthcare evolves and networks become “smarter,” areas of population specialization will continue to grow. It is the responsibility of industry leaders to voice concerns about the risk adjustment of Quality Measures that are used for the purposes of public reporting. As these measures increase in number, and grow in importance in the eyes of payers and the public, any inherent bias should be avoided — and if it’s not, then clearly communicated in a way that allows for transparent and fair comparisons.
The survey process needs to be evaluated for its flexibility in assessing facilities that care for atypical populations. Ultimately, Five-Star should be recast to account for the uniqueness of people being cared for in SNFs.
In the meantime, providers caring for specialty populations must learn to use their data to demonstrate that they are 1) different, 2) meeting a need within their community and 3) achieving positive outcomes, despite what the public data might suggest.
Thankfully, that SNF I mentioned is, on a local level, acknowledged as an excellent provider of care for this challenging population and they are sought after by many “smart networks.”
Steven Littlehale is a gerontological clinical nurse specialist, and executive vice president and chief clinical officer at PointRight Inc.





