
I asked all the leadership at New Choice Nursing and Rehabilitation Center to bring me their department-specific resident assessment tools. They were to leave them on my desk by 5 p.m. When I returned the next day, I got to work picking through the considerable stack of tools and categorizing them into the specific resident system that each assessed.
My work was easy, quick and transparent. Within an hour I’d begun pasting the facility-required assessment tools on the wall, categorizing them by resident functional system. Three assessments for cognition were on the left, two assessments for ADLs in the middle, three for mental wellness on the right, two for pain on the opposite wall … you get the idea.
When I was done, the wall had more layers of paper on it than a Victorian farmhouse. Sadly, and not surprisingly, the MDS was nowhere to be seen — not on the wall, not in conversation, never a consideration, ever.
I was hired by New Choice to streamline their workflow, make them more efficient and improve their outcomes. But all that organization I’d done ended up being in vain. As soon as I shared my results and recommendations to eliminate assessments/documentation and embrace a more interdisciplinary model of care, my engagement was abruptly terminated.
Looking back, it’s not hard to understand why. I was young, most certainly cocky, and I’d just called their baby ugly. I had poked at their culture and challenged processes that were put in place by a beloved DON, three DONs ago. Removing and simplifying processes was not in that facility’s nature, and I have learned through the years that they are not alone.
Is there something uniquely human that disinclines us from choosing a simpler, more efficient process? Is adding to a process or regulation valued more than stripping elements away? A recent article from the journal Nature seems to bear that theory out. Researchers reported that a series of problem-solving experiments demonstrated that people were more likely to consider solutions that added features than solutions that removed them, even when removing features would serve them best. The Washington Post covered this story here.
With this in mind, can you fathom the challenge that every new Centers for Medicare & Medicaid Services administration faces? They must immediately solve for [insert problem] and demonstrate success by [insert specific time before next election]. In my Walter Mitty fantasy, I envision bureaucrats peeling off regulation-lined conference room wallpaper, flipping the paper over, and exclaiming “Look, I got one from the early ’70s!”
The last administration launched the Patients Over Paperwork initiative, which reported a $6.6 billion ROI by this year’s end. The current administration instituted the Office of Burden Reduction & Health Informatics, whose focus is to “reduce administrative burden and advance interoperability and national standards.”
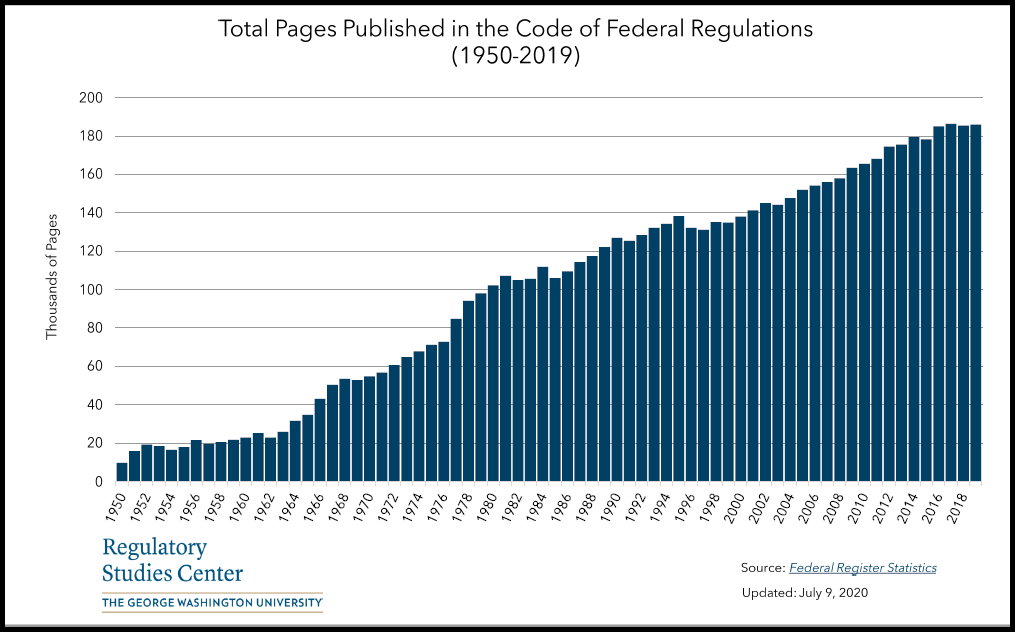
Yet despite these individual efforts to remove red tape, statistics speak for themselves. George Washington University put together the above graph that tracks the volume of the Code of Federal Regulations from Harry Truman’s presidency to now. If history is the best predictor of the future, we’ll likely see more complexity, not less.
Steven Littlehale is a gerontological clinical nurse specialist and chief innovation officer at Zimmet Healthcare Services Group.
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.





