An expanding coronavirus pandemic continues to devastate the long-term care sector on numerous fronts. Operators are being pushed as never before to deliver care while underequipped, understaffed and pressed to admit infected patients, a new McKnight’s Flash Survey reveals.
The Round 2 McKnight’s survey found that the percentage of provider respondents with COVID-19 detected in their buildings had nearly doubled (to 34%) within two weeks.
In addition, nearly 1 in 6 (16%) had had a resident or worker die due to COVID-19, while more than 1 in 5 (21%) had had residents move out due to COVID-19 fears.
Extrapolating the statistics to a nationwide total of about 16,000 skilled nursing facilities, the numbers could indicate that more than 5,400 nursing homes have had COVID-19 detected in their buildings. In addition, 2,600 facilities might have already experienced at least one coronavirus-related death and more than 3,300 having at least one resident leave due to COVID-19 or fears of the virus. There has been no national strategy or mandate for reporting nursing-home related COVID-19 infections or deaths, though federal health officials said they planned to announce one this week.
McKnight’s collected the latest survey results from 631 respondents following an email sent to the publication’s readers on Tuesday and Wednesday of this week. As an incentive, McKnight’s offered participants the chance of being entered in a drawing for a $50 gift card..
Workforce challenges
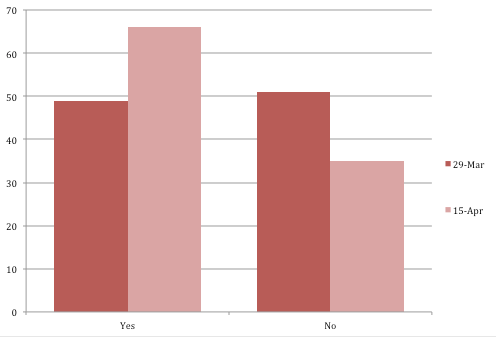
COVID-19 concerns?
Results of the survey show a profession facing far more workforce challenges than usual. Two-thirds of respondents (67.4%) said they had staff call in sick or quit due to COVID-19 concerns, up from 45% in a McKnight’s survey two weeks earlier.
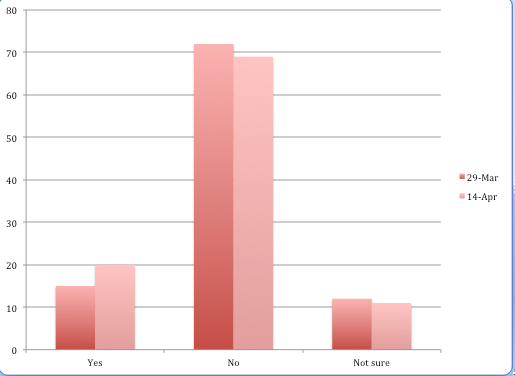
More than 83% said they were using homemade or reused personal protective equipment, significantly up from 55% in the first survey.
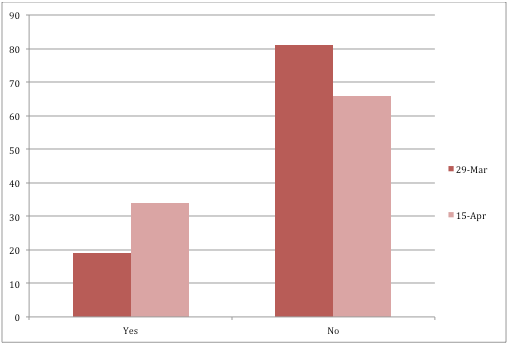
A total of 19.8% of respondents said they felt pressure from hospitals to admit patients who had been treated for the coronavirus, up by nearly half from 14% two weeks earlier.
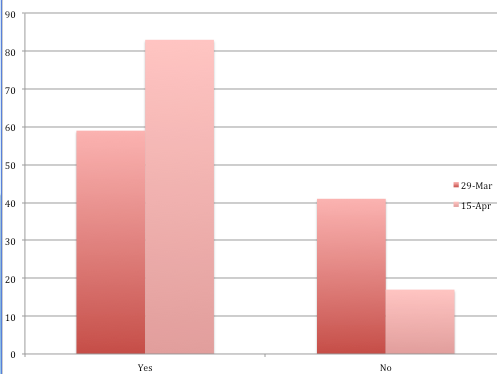
or reusing PPE?
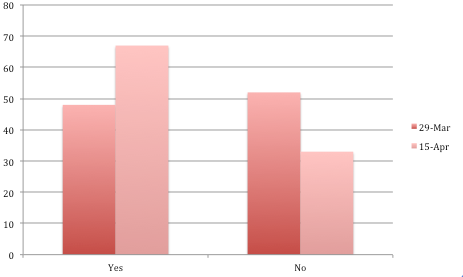
Toughness growing
The trait of resilience also revealed itself in the survey responses, with 64.6% of participants saying they were equipped to handle COVID-19 patients, up nearly 15 percentage points from two weeks ago. The percentage of those reporting PPE shortages actually fell slightly (to 71% from 75%), perhaps a reflection of the huge rise in the use of homemade or reused equipment.
Given the option of checking as many choices as applied at their facilities, the vast majority of respondents described the mood in their facilities as “Coping day to day” (63%) or “A little shaky but confident overall” (55%). That tracked closely with two weeks earlier, when the numbers were 59% and 46%, respectively.
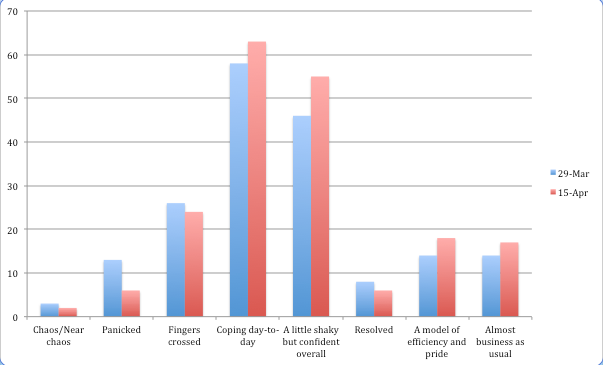
And the mood among respondents at nursing facilities seemed to remain steady over the last two weeks, a period when the number of cases and deaths soared in the U.S., and in the long-term care population in particular. On Wednesday, COVID-19 deaths connected with long-term care facilities reportedly were at least 5,500, which didn’t include statistics from many states that said they didn’t keep them.
Next in line again was “Fingers crossed” (24%, down from 26%), while the more confident choices of “A model of efficiency and pride” (18%) and “Almost business as usual” (17%) grew from 14% for each two weeks earlier.
On the fringes of the less-confident range, those responding “Panicked” fell to 6% from 13%, while “Chaos/Near chaos dropped to 2% from 3%.