The nation’s nursing homes are heading into the toughest days of the COVID-19 outbreak both underequipped and understaffed, according to results of an exclusive McKnight’s Long-Term Care News flash survey.
More than 77% of respondents said their facilities were experiencing personal protective equipment (PPE) shortages. Nearly 3 in 5 (59%) said their locations were using homemade or improvised PPE, or reusing it. Masks, gowns, gloves and shoe covers are just some of the infection control products falling under the PPE label.
In addition, nearly half of the respondents (48%) said they have workers “calling in sick due to or exhibiting signs of COVID-19.” This is on top of normal staffing concerns that leave many facilities scrambling to fill open shifts.

Survey results reflect a distressed industry seeking answers to challenges that could grow by the day. The number of U.S. hospitalizations is surging by thousands per day, putting more stress on the entire healthcare continuum, particularly nursing homes, where the individuals most at risk of falling prey to the highly contagious, deadly virus live.
More than 19% of survey respondents reported that COVID-19 had been detected in at least one resident or worker at their facility. The survey did not explore how many more had personnel quarantined or suspected of being COVID-positive.
Over half (51%) of the survey respondents said their buildings were not currently equipped to handle COVID-19 patients. This comes at a time when numerous states are contemplating whether to follow New York’s lead of mandating that nursing homes accept any patient discharged from a hospital in the state, including individuals treated for coronavirus.
More than 15% said their facilities already had been pressured to admit COVID patients from the hospital, while 72% said they hadn’t and 12% weren’t sure.
Staffing challenges
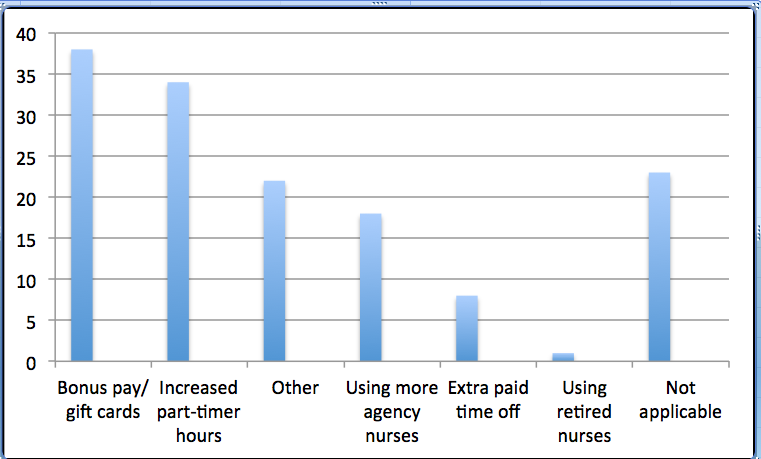
Managers said they were compensating for extra staffing needs with a variety of incentives and resources. “Bonus pay/gift cards” lead the way at 38%, followed by “increase part-timers’ hours” at 24% and using more agency nurses (18%). More than 22% entered something in the “other” category, which included flex-time, regular or special overtime pay, and managers filling in for staffers as the most popular choices. More than 23% said a question about “compensating for extra shifts/other staffing needs” was “not applicable” to their facilities’ situation.
A majority, however, observed some kind of anxiety among staff. “Coping day-to-day” was the top choice (59%) when asked “How would you rank the overall mood in your building?” That was followed by “a little shaky but confident overall” (46%) and “fingers crossed” (26%).
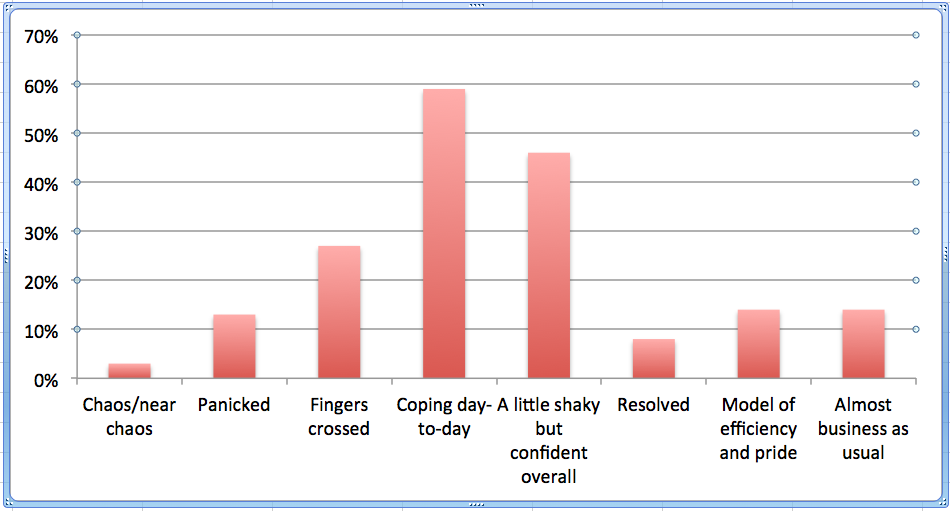
About 1 in 7 (14%) labeled their building’s mood as either “a model of efficiency and pride” or “almost business as usual.” On the other end of the spectrum, 13% characterized the mood as “panic” while 3% called it “chaos/near chaos.” Participants were encouraged to choose as many options as they felt were applicable.
Whatever uncertainty or worries survey results revealed, they also exposed a huge wave of creativity to “keep spirits up.” More than 80% of respondents shared strategies their facilities were undertaking to improve the mood. The most common involved free meals or snacks, dress-up/theme days, motivational talks, and increased communication and verbal appreciation.
Survey participants comprised 350 McKnight’s Long-Term Care News readers who responded to an email blast Saturday or Sunday asking them to take part in a survey seeking their views on the virus’s effects on their nursing home or skilled nursing operations. Participants were entered in a random drawing for a $50 gift card.
The biggest group identified themselves as owners, operators or administrators. Nursing leaders and a category for “other” (29% each) came next. The latter group consisted of CFOs, HR directors, medical directors, pharmacists, therapy leaders and other top managers.
Stay tuned to mcknights.com and mcknightseniorliving.com for ongoing COVID-19 developments and how they affect long-term care and senior living providers.



