
COVID-19 cases in U.S. nursing homes have hit their lowest mark since federal officials began tracking last May, according to a new report issued by the American Health Care Association and National Center for Assisted Living Tuesday.
The report is based on Centers for Medicare & Medicaid Services data through March 7. In addition to showing a 96% decline in nursing home cases, it indicates COVID-19 related deaths in nursing homes declined by 91% since December 20.
But the good news comes as COVID-19 cases are surging nationwide, fueled by variants and a pullback on mask mandates and social distancing restrictions.
And some nursing homes indicate they are also struggling to maintain access to vaccine supply now that an initial federal program has ended.
“We are not out of the woods yet, but these numbers are incredibly encouraging and a major morale booster for frontline caregivers who have been working tirelessly for more than a year to protect our residents,” said Mark Parkinson, president and CEO of AHCA/NCAL. “This trend shows that when long-term care is prioritized, as with the national vaccine rollout, we can protect our vulnerable elderly population.”
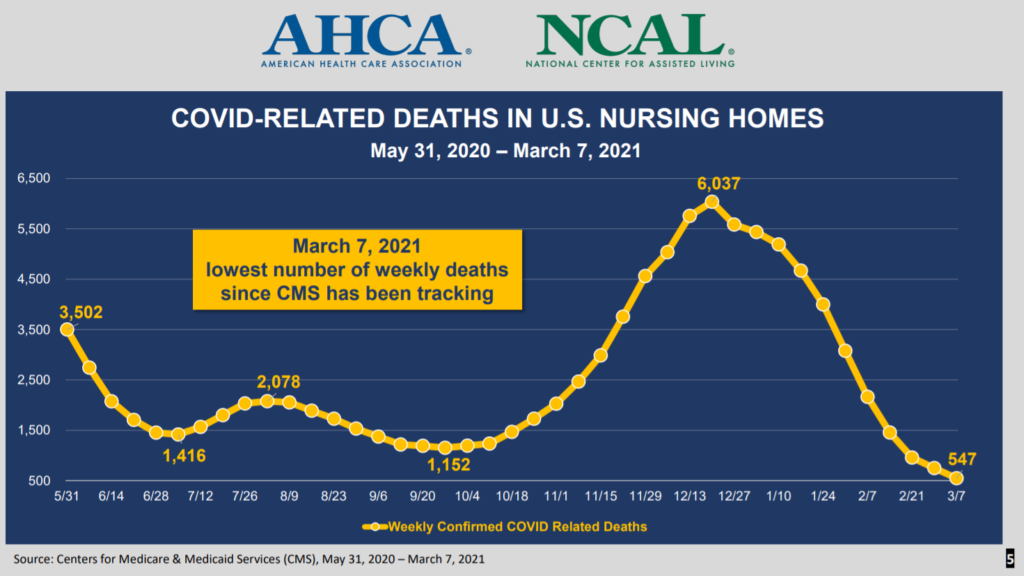
For the week ending March 7, nursing homes reported 547 deaths nationwide, down from 6,037 during the peak week ending Dec. 20. That was around the same time federal officials launched a coordinated effort to supply COVID-19 vaccines to all nursing homes in the country.
As of Tuesday, the Centers for Disease Control and Prevention reported at least 2.1 million long-term care residents had received at least one COVID-19 vaccination dose. That figure includes residents of assisted living facilities.
The federal campaign, however, has all but ended for nursing homes, leaving states to create a patchwork of vaccine access programs that ensure shots continue to get into the arms of new residents and staff members.
Some state leaders have found too few long-term care pharmacies to step up and provide a distribution network, while others say individual facilities have failed to sign up for specific programs designed to provide continuity.
“We’re hearing that (ongoing access) is getting better, but it’s something we’re keeping an eye on,” AHCA said in a statement Tuesday. “Recently, we have seen some vaccine allocated to long-term care, but we need to remain vigilant and keep long-term care residents and staff a priority as everyone’s attention shifts to the general population.”
All of this comes as public health officials have become more concerned about emerging variants. They see the race to vaccinate as a key way to keep new strains from endangering the public, including vulnerable seniors.




