
Nearly all for-profit nursing homes, which account for two-thirds of US facilities, would need to hire more nurses to meet provisions of the newly proposed federal staffing mandate, results of a new analysis Monday revealed.
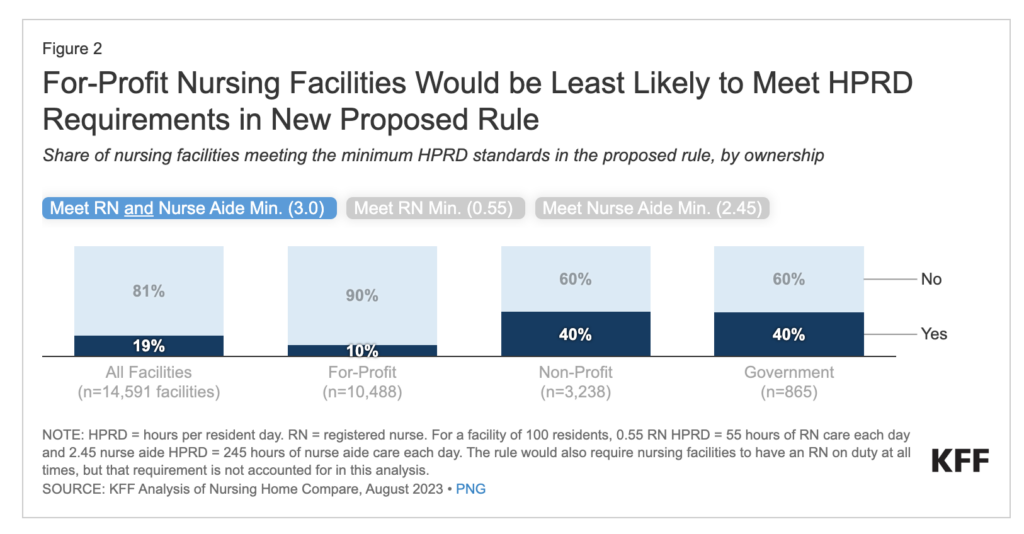
While 90% of for-profits would have to hire staff, that level is just 60% on the nonprofit and government-run side, a KFF breakdown of projections showed.
“The data reinforces two truths: nursing homes are not all the same …,” said Katie Smith Sloan, president and CEO, LeadingAge, which represents nonprofit providers of aging services. “The workforce crisis is real. Nurses are in short supply — and not just in nursing homes. CMS’ proposal raises very real challenges for the whole health care sector. The end result is older adults and families’ access to care is in jeopardy.”
Most provider groups have been sounding warnings for more than a year about the national staffing crisis and how facilities would be impacted if the Centers for Medicaid & Medicare Services moved ahead with a staffing rule.
The proposed rule was released Sept. 1 and would give facilities at least three years to provide a minimum of 3.0 hours per patient day of direct care — 0.55 hours of that by a registered nurse and 2.45 hours by a nurse aide. Non-rural nursing homes would have three years to comply with some elements of the rule, with rural facilities given five years to get up to speed on the overall hourly rate. A requirement calling for 24/7 RN coverage, triple the current standard, would go into effect two years after the rule is finalized for urban providers, with another year granted to rural providers.
The proposal also includes options for hardship waivers and $75 million for training for nursing aides.
According to KFF’s analysis, if the staffing rule went into effect today, just 19% of facilities would be in compliance. Just more than that half – 52% – would need to hire more RNs and 72% would have to hire more nurse aides. CMS estimated that 25% of facilities would meet the minimum staffing requirements, but KFF noted that that estimate did not account for the 24/7 RN rule.
“It is not clear how CMS accounted for the 24/7 rule given currently available data or what month(s) of data were used in the CMS estimates,” the KFF authors wrote. “KFF uses the most currently available data for both RNs and nurse aides. Different months of data could also contribute to differences in the estimates. Neither KFF nor CMS account for the hardship exemptions in the estimates, nor is it clear what share of the facilities that do not meet minimum standards would apply and qualify for a hardship exemption.”
In particular, KFF warned that waivers already available for RN hiring hardships might make the effects of the proposed rule on minimum staffing levels “muted.”
CMS’ proposal said that it would identify LTC facilities that needed a higher level of staffing, depending on patient characteristics so that nursing homes with residents with more complex health or functional needs would need more staff. CMS is asking for feedback on whether it should use case-mix adjustment when determining compliance or rely on self-reported hours of care.
“Specifically, among 14,591 facilities, only 38 facilities would meet requirements when using a case-mix adjusted staffing level since most facilities’ case-mix staffing levels are lower than their reported staffing levels,” the analysis noted. “Just 4.2% of facilities would meet the requirement for RNs and 0.3% would meet the requirement for nurse aides if staffing requirements were adjusted for resident heath and frailty characteristics.”
A statement from the American Health Care Association/National Center for Assisted Living emailed to McKnight’s Long-Term Care News on Monday took the federal proposal to task.
“This report further confirms what we’ve been saying: this unfunded mandate will be impossible to implement,” the statement said. “When more than half of the industry, regardless of ownership, is unable to meet these requirements, that speaks volumes to how deeply flawed the policy is. … The Biden Administration’s proposal offers no meaningful support to help build a pipeline of new caregivers or incentivize them to choose a career in long term care. There needs to be a comprehensive investment to strengthening the long-term care workforce, not unfunded mandates. We hope to convince the Administration to never finalize this rule as it will only worsen access to care for our nation’s seniors.”




