
Waivers of a 3-day stay requirement for patients covered by accountable care organizations did not lead to more bad outcomes or lengthen nursing home stays, a federal analysis has found.
The 58-year-old minimum stay rule mandates that patients be admitted to a hospital for at least three consecutive in-patient days to trigger Medicare coverage of follow-up skilled nursing care. But the Centers for Medicare & Medicaid Services has been testing waivers of that rule, notably as a way to ensure patients have had access to care during the pandemic.
The agency also has waived the requirement for some Medicare Advantage plans and shared savings plans through its Center for Medicare & Medicaid Innovation.
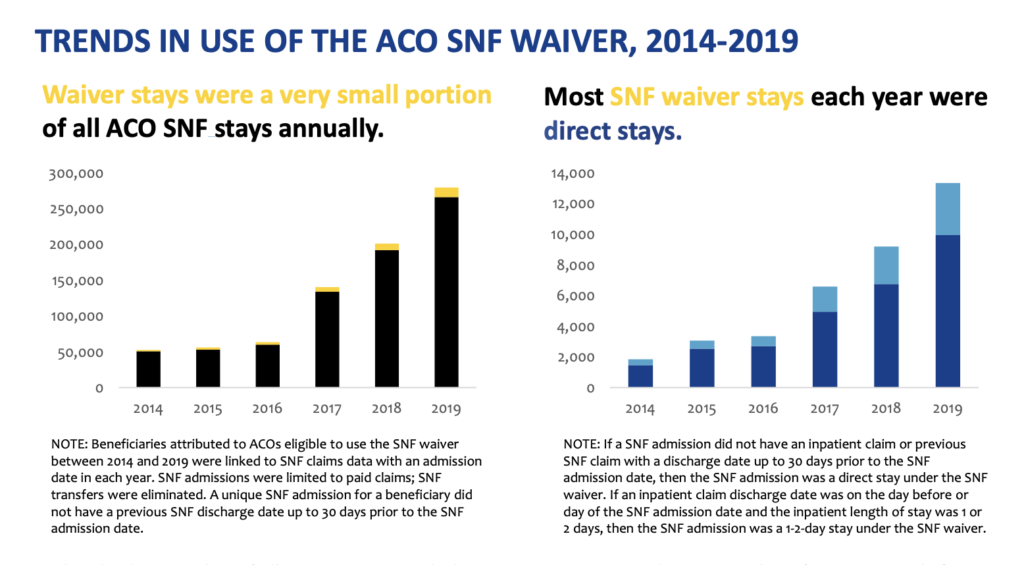
The innovation center published the February analysis, which showed that use of the waivers grew among ACOs between 2014 and 2019. Most plans relied on them to allow patients direct access to a nursing home with no hospital stay at all.
“Two potential concerns with the use of the SNF waiver were whether ACOs would increase Medicare costs by increasing SNF length of stay or use the waiver to convert community-dwelling beneficiaries to long-stay nursing home residents,” CMS reported. “Both concerns were not evident in ACOs’ use of the SNF waiver. SNF length of stay and long stays decreased and discharges to home and home health care rose.”
A growing number of ACO plan types could elect to use waivers over the study period, but the waiver was still used in just 3% to 5% of all SNF stays each year. Fred Bentley, managing director at ATI Advisory, told McKnight’s Long-Term Care News on Friday that level was within range of the usage typically reported by Medicare Advantage plans.
Among ACOs, patients were more likely to be referred to a SNF with a waiver from home rather than after a 1- or 2-day hospital stay.

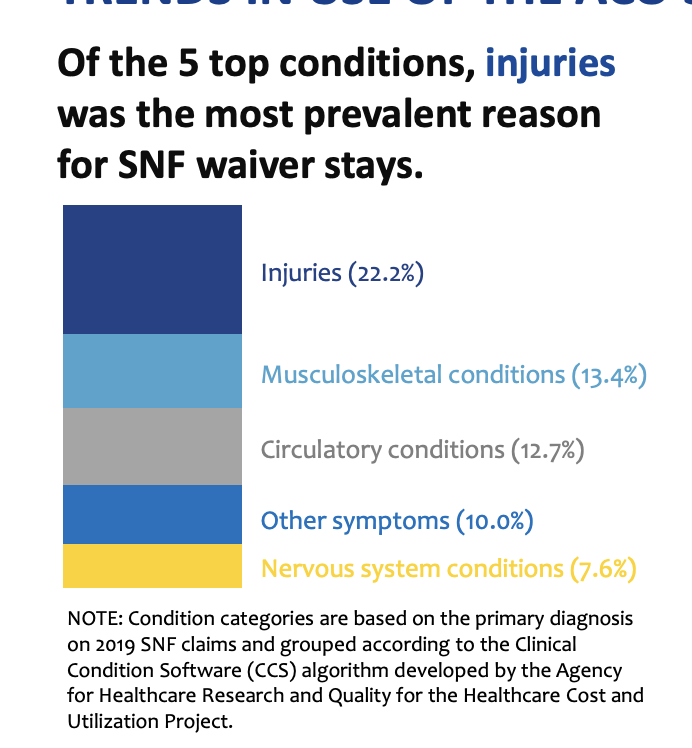
Patients most likely to receive a waiver had an injury (including a fall or dizziness); musculoskeletal condition, circulatory conditions, “other” symptoms, or a nervous system condition.
“This [analysis] demonstrates there’s a value to having SNFs as an option and an alternative to in-patient admission,” Bentley said. “I think the sticking point is still there, from a policy and regulatory standpoint, which is that this is a very controlled environment where the ACOS and the physicians in the ACOs are making the decisions about who gets admitted, when they get admitted and who goes to the SNF.”
Many other patients likely could have received waivers, CMS said, but providers in the ACOs did not pursue them. That led the agency to conclude that lower adverse outcomes were driven by patient selection.
ACOs are also only allowed to use waivers at skilled nursing facilities with ratings of 3 stars or higher.
Providers want chance to replicate outcomes
While many patients in ACOs and Medicare Advantage plans will continue to have some access to waivers after the public health emergency ends on May 11, there is no alternative for the roughly 50% of beneficiaries still covered by traditional Medicare.
They will go back to being denied post-acute coverage without a 3-day stay.
It’s among the broader Medicare population, where fewer intermediaries are in play, that CMS would have more trouble ensuring that SNF stays aren’t used too often without a preceding hospital admission.
“The concern is if you were to lift the waiver entirely, get rid of the 3-day stay for the entire Medicare fee-for-service population, what could potentially happen in terms of skilling in place and the incentive nursing homes would have to flip patients,” Bentley noted.
During the pandemic, nursing homes have been vital partners to hospitals filled to capacity. The 3-day stay waiver freed up much-needed hospital beds faster, and it also likely lowered the overall cost of care by moving patients to a non-acute setting more quickly.
The waiver’s success united providers, families, consumer groups and some lawmakers around lifting the requirement permanently. Federal legislation introduced in summer 2021 would have allowed observation stays to count toward the required days requirement, but it did not pass.
Providers in the last few weeks have clamored for a permanent change.
LeadingAge President and CEO Katie Smith Sloan on Feb. 16 wrote to Congressional leaders and Health and Human Services Secretary Xavier Becerra demanding the waiver be made permanent until Congress acts to repeal the rule altogether.
She referred to previous audits conducted by Medicare Administrative Contractors since 2020 that show that waiving the rule has had no negative effect on patient outcomes, and also has not led to an increase in inappropriate admissions. CMS also could have rescinded the waiver at any time if it had proven ineffective, which it did not, she reasoned.
“Millions of dollars in unnecessary health expenses” have been rung up due to the rigid three-day stay mandate, Sloan wrote. “Lengthening hospital stays is duplicative, costly, and perhaps most importantly, confusing and challenging for older people, particularly those with cognitive impairments.”
Last week, CMS SNF team lead John Kane reiterated to providers on a national stakeholder call that the 3-day stay rule’s statutory basis requires Congressional action for any change to happen.
Though Bentley said a permanent fix could build in protections for patients and disincent abuse. Attaching conditions that only allow highly rated facilities to care for non-hospitalized patients or limiting conditions for which the rule could be permanently waived might work.
“They would certainly be scrutinizing that,” Bentley said. Congress could “authorize CMS to track that very closely and look at facilities that have higher-than-normal skill-in-place rates, dig into that and control for quality.”




