

The state government’s response to the earliest days of the COVID-19 pandemic left New Jersey nursing homes confused and without adequate supplies, according to a new independent analysis.
The report also called for more sustaining funding for providers — making special note how such investments could be used to increase wages, staffing and preparedness for future emergencies.
The more than 900-page analysis from the New Jersey firm Montgomery McCracken Walker & Rhoads highlighted a March 2020 directive from the state Department of Health that nursing homes should admit residents even if they were sick with COVID.
While intended to keep hospital backlogs manageable, the rapid progression of the pandemic forced the state to quickly reverse that directive two weeks later. Former New York Gov. Andrew Cuomo came under blistering attacks for a similar policy and reversal in 2020.
The report also confirmed that hospitals were given priority for masks and other protective gear — a policy that would leave nursing homes and their frail patients in short supply of those vital items.
These were key examples of an overall lack of preparation and resources in the pandemic’s earliest days and how they hampered the providers’ emergency responses.
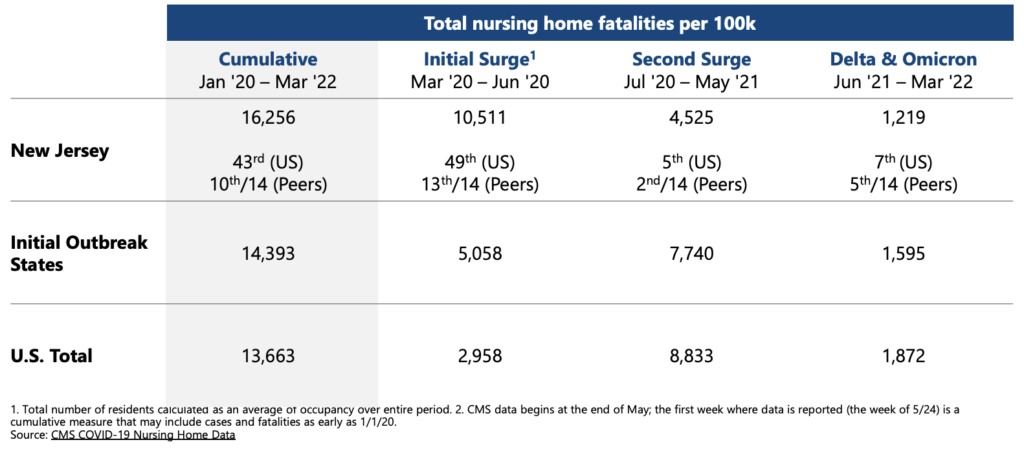
While the state’s performance improved later in the pandemic, such early missteps contributed to New Jersey having the second-worst rate of nursing home deaths in the nation between March and June 2020.
While noting the good intentions and the eventual improvements of state agencies’ performances, authors Paul Zoubek and Montgomery McCracken called for better planning for the future in the report’s dedication.
“Neither the State nor the Federal Government had clear, executable plans in place,” they wrote. “We hope the report can serve as a playbook for New Jersey — a guide to putting in place the appropriate resources, plans, and processes — so that we can all be better prepared for the next major crisis.”
A key step for that future readiness would be increasing the funding that government invests in healthcare providers.
“An overarching theme that emerged in many different contexts was that the public health system requires ongoing investment,” the authors explained. “It cannot be ignored or underfunded for years and then be expected to become capable of handling a massive global crisis. An effective public health capability requires substantial and consistent financial support, including adequate staffing and compensation that attracts people with the necessary knowledge and skills.”
Such funding would be welcome news to long-term care providers, who have struggled with healthcare’s highest turnover and vacancy rates for years.





