
Advanced practice clinicians who specialize in skilled nursing care help reduce the use of unnecessary care at end of life, according to new study results released Friday in JAMA Network Open.
These physicians, nurse practitioners and physician assistants — who provide at least 80% of their evaluation and care visits in nursing homes — were referred to collectively as “SNFists” by the report authors. They reduced the burdensome care transitions that many residents face, benefiting both caregivers and their patients, the study confirms.
More than 20% of the patients studied experienced at least one burdensome care transition during end-of-life care.
Other studies previously established SNFists’ positive impact on long-term care hospitalizations, antipsychotic drug use and other issues, but this is the first to highlight their impact on end-of-life care quality, study authors noted.
Providing excellent end-of-life care is especially challenging for providers due to the additional training necessary, the different care priorities sometimes required by patients, and the staffing and funding issues.
The fearsome foursome
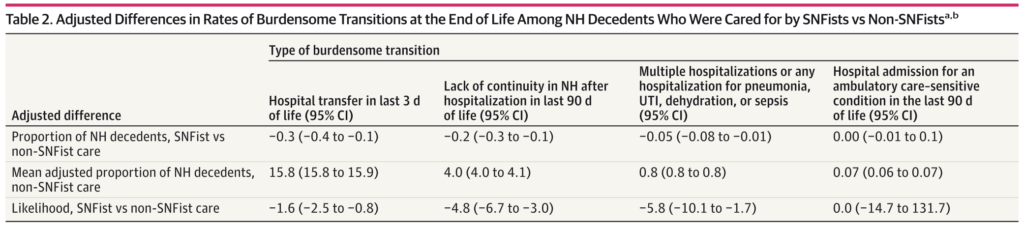
The JAMA study focused on four “burdensome” care transitions: hospitalizations in the last three days of life; being transferred to a different nursing home after a hospital stay; being rehospitalized for the same issues or hospitalized at all for a relatively minor issue; and hospitalization for an ambulatory care-sensitive condition.
Residents who received care from SNFists reduced the risk of three of the four care transitions studied. Only ambulatory care-sensitive hospitalizations did not improve.
A June 2023 study showed that the prevalence of SNFists in nursing homes exploded from only 13.5% in 2013 to 52.9% in 2018. The JAMA study noted that SNFists are more likely to be present in larger, for-profit nursing homes.
SNFists were particularly adept at preventing residents from being discharged to an unfamiliar nursing home (about 5% less likely) and being hospitalized multiple times or for minor issues (about 6% less likely).
Dementia care implications
The authors noted that most nursing homes already use SNFists to some degree. They said the trend should be accelerated.
“Although further research is required to better characterize the mechanisms and the degree to which SNFists provide holistic care across various domains,” the authors stated, “there are several policy implications that can be drawn from these findings…. Our findings underscore the growing importance of SNFists in the delivery of EOL care to frail US individuals with advanced age and associated comorbidities, particularly those with dementia, as two-thirds of all deaths related to Alzheimer disease occur in NHs.”
The authors also noted that most of the growth in SNFists is among advanced practitioners and there may be an unmet need for physicians specializing in nursing home care. Medical schools and residencies should provide more training and pathways into nursing homes to meet this need, they added, noting that such training also should be provided to nurse practitioners and physician assistants.
Finally, because so many nursing home residents experience burdensome care transitions, the authors recommended a broad, collaborative push from nursing homes, payers and policymakers to reduce those experiences.





