
Xavier Becerra, U.S. Secretary of Health and Human Services
Less than a day after President Biden declared May 11 will be the end of the public health emergency (PHE), nursing home leaders were scrambling to understand the full implications, while also making plans to fight the return of some less flexible conditions.
The top concern is coping with the return of the three-day stay provision. A campaign is already under way to make the current waiver for it permanent.
Other stakeholders are most concerned about the redetermination process for thousands of Medicaid beneficiaries. They must smoothly receive notifications and apply to federal health officials properly to receive proper Medicaid coverage.
Also of note will be the expiration of the Spell of Illness waiver, which figures to affect far fewer patients than the above two conditions but still remains hot on providers’ radar.
Prior to Monday’s revelation, federal health officials had already peeled back most of the waivers spurred by the pandemic, noted experts in discussions with McKnight’s Long-Term Care News Tuesday. That diluted the potential drama of the PHE expiration date announcement for many. But not top nursing home lobbyists.
“The PHE may be ending, but there is more work to do to address the challenges spurred by the pandemic,” said American Health Care Association President and CEO Mark Parkinson. “Long-term care is now facing a historic labor and economic crisis, and we need meaningful, supportive solutions that will help us rebuild.”
LeadingAge President and CEO Katie Smith Sloan added that long-term care operators may again find themselves on the hot seat, even if the general public doesn’t share the same dangers or concerns. It’s a scenario not unlike the start of the pandemic.
“The rest of the world may be moving on, but for our members, the costs and complexities from the pandemic are ongoing,” she cautioned in a statement to McKnight’s.
Giving providers more than 100 days to plan for the PHE closeout — well beyond the 60-day minimum span Health and Human Services Secretary Xavier Becerra (pictured) had promised — is helpful, Smith noted. But that may just mean a break before some really painful days hit, she added.
“[O]ur members are severely overstretched and now face a new landscape of funding and rules while simply trying to survive,” Sloan said. “Questions still remain not just about waivers and flexibilities, but policies and other aspects of how the Biden administration will shift gears to a true post-COVID country. We are actively reaching out to CMS, HUD, and other agencies to better understand what their plans are.”
Chipping away at rules
The Centers for Medicare & Medicaid Services has slowly stripped back many of the waivers instituted after the pandemic was declared three years ago. Among those have been certain physician visit requirements, for example.
The end of the PHE will bring a close to the Section 1135 National Blanket Waiver, which notably involves the Medicare fee-for-service three-day stay and Spell of Illness waivers. The first is a requirement for Medicare coverage and the second allows extra coverage without as many stipulations. Last year, Medicare Advantage plans rolled them back.
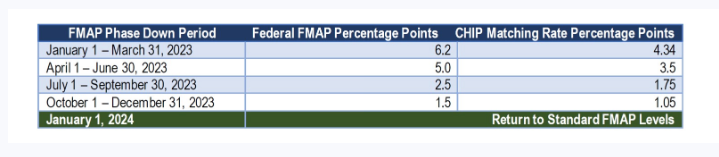
Ending the PHE will impact Medicaid rate add-ons attached to it, AHCA noted in a blog post Tuesday. However, the sector is happy that the 6.2% Medicaid Federal Medical Assistance Percentage (FMAP) increase was detached from the PHE, so its expiration will not harm that rate boost. Instead, it is now amid a year-long phase down, as illustrated in this chart:
Temporary nurse aide statewide waivers also may be affected. CMS may extend them until May 11 if sufficient need is shown. Currently, 18 states now have them in play, with expiration dates between March 20 and April 7.
In addition, Congress more recently extended extra telehealth flexibilities until Dec. 31, 2024, noted Cynthia Morton, executive vice president of Advion.
Morton, however, is not sold on regulators’ moves.
“Maybe losing the PHE is a recognition for much of society that we are moving to a normal, but for long-term care, this is not really the case,” she told McKnight’s Tuesday. “Long-term care is very short of staff in nursing, therapy and other positions. I don’t know that we have seen full recognition of this problem by policymakers, and the solutions are not very easy. Policymakers taking money out of our sector will not help us address this workforce shortage.”
Enrollment worries
The Medicaid redetermination process has some state association executives, including Ron Nunziato of the Health Care Council of Illinois, most concerned. The fact that managed care companies will oversee some of the selection and notice-delivery processes doesn’t help, he added.
“Probably the biggest angst operationally is the redetermination periods,” said Nunziato, a provider executive for 29 years before joining HCCI last year. “You don’t really know if your residents got their letters, and if they did, what they do with them.
“It will take 12 months to get through the redetermination process,” he added about Illinois’ plans, which have been in the works for months. “That has everyone on pins and needles. People have been gearing up to process notices so no one is waiting for the determination letter and gets cut off. We have to make sure systems are in place and work.”
Because of such high employee turnover in the sector, he advised operators to start educating staff who may have never dealt with the redetermination or three-day rule processes before.
“Those who did it before might have forgotten about it, and some people are new to the sector altogether,” he noted. “Providers have to do these every year. Start meeting with all families and residents to start data gathering to get through this.”
He, like all other leaders interviewed for the article, couldn’t think of anything good to say about the PHE being retired. But he did have additional concerns, such as the worry that the general public will relax its infection control practices and precautions.
“COVID has been tamed, but it hasn’t been eradicated,” he said, repeating a phrase he says he often uses to remind of ongoing COVID concerns.
‘We’re past the worst’
The problems of getting enough staff or rebuilding census also have not been eradicated, pointed out Rick Matros, CEO of Sabra Healthcare REIT. That’s why the last few of the 12 PHE extensions have been especially helpful, he told McKnight’s in an interview Tuesday.
“We [the sector] needed to make more progress on recovery and these last months have brought that, though we [Sabra] probably still are 400 to 500 basis points below pre-pandemic occupancy levels,” Matros said. “And the margins are even worse because of the labor market.”
He said he’s been telling investors that Sabra might have to “step up and help operators on a temporary basis with rent for a few months.”
“We may have to buy people some more time. But we’re past the worst,” he added.
The exception could be smaller, lesser capitalized operators, he explained. Others have predicted that smaller players could be pressured from the market if they cannot hang on until conditions improve.
Matros said the three-day stay waiver might not be as pivotal now as it was earlier in the pandemic, but it still deserves to be made permanent.
“It’s good public policy and it’s good to have because COVID variability could go up again,” he explained. “And hospitals, who have always been against the three-day rule waiver, have really seen how this makes nursing homes better partners.”
Waiving the rule makes good fiscal sense, too, claims Melissa Brown, the Chief Operating Officer of Gravity Healthcare Consulting.
“We have learned through this pandemic-induced experiment — the nationwide three-day stay COVID waiver — that the three-day stay really isn’t necessary and is a barrier to effective, lower cost care that can be provided in skilled nursing,” Brown told McKnight’s Tuesday. “Legislators and CMS should take note and should do away with an archaic policy that increases costs but does not improve quality and does not serve the patient best.”
Brown said that providers should double-down on staff education on the three-day stay waiver since apparently it will soon be back in play.
“You have probably turned over most of your staff in the last few years while this waiver was in effect,” she noted. “So make sure your team understands how and when to send patients to the hospital for an appropriate three-day stay so that they can become eligible for skilled services when that applies.”




