
If there’s anything that will bring a bipartisan group of U.S. senators together, it’s the topic of abuse in nursing homes and a hearing Tuesday was proof yet again.
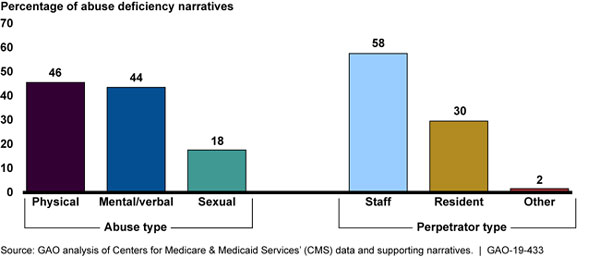
Abuse deficiencies cited in nursing homes more than doubled in four years, increasing from 430 in 2013 to 875 in 2017, a Government Accountability Office report released Tuesday found. The most common physical and verbal abuse was by staff, at 58%, investigators said.
Members of the Senate Finance Committee, however, directed much of their ire not at providers but rather at the Centers for Medicare & Medicaid Services.
“Not only have abusive incidents doubled in recent years, but the GAO has found that CMS – the agency charged with ensuring that these facilities meet federal quality standards – often cannot access information about abusive incidents after they occur and, therefore, cannot take the necessary steps to remedy the situation,” said Sen. Thomas R. Carper (D-DE).
“CMS needs to ramp up its oversight efforts and fix the problems identified by the Government Accountability Office,” added Sen. Charles Grassley (R-IA), the chairman of the committee.
Common ground
All parties at the hearing — which included American Health Care Association’s President and CEO Mark Parkinson — stressed a need and commitment to reducing abuse and neglect in nursing homes. They all also found common ground on better background check practices.
“Our members need access to the National Employee Data Bank so we can learn when potential employees with criminal backgrounds have moved across state lines. We don’t have this information and we need it,” Parkinson said.
Ranking committee member Sen. Ron Wyden (D-OR) expressed surprise that 13 states have no background check process for nursing home employees.
There are inconsistencies and loopholes throughout the country when it comes to nursing home oversight, including about providers having to self-attest their ownership, testified Megan H. Tinker, Senior Advisor for Legal Review of the Office of Counsel to the Inspector General, Health and Human Services.
Additionally, a provider can be eligible for Medicaid if it is already in the Medicare program, even if there hasn’t been a background check through Medicare, Tinker added.
“That leaves open a possibility a provider could be a provider for Medicaid with no background check,” she said, adding that CMS did not concur with that recommendation to close that loophole.
Funding concerns
Despite agreement on needing to reduce abuse and neglect, policy makers and experts differed on the best way to achieve those goals, specifically when it comes to funding.
“Medicaid covers two out of three nursing home residents. We need to strengthen Medicaid,” said Sen. Debbie Stabenow (D-MI).
In response to a question about mandatory staffing from Sen. Catherine Cortez Masto(D-NV), AHCA’s Parkinson harkened back to his days running nursing homes, acknowledging that more workers is generally better but also how it depends on how careful and efficient a given certified nursing assistant is.
He also noted that in order to achieve a higher ratio of staff to residents of 4.1 hours per resident per day, as some have suggested, it would cost potentially an additional $6 billion.
“If there’s a mandatory staffing requirement that would be paid for, we’d be all for it,” he said. “But if it’s not paid for, there is no practical way to do it.”
Lori Smetanka, Executive Director of the National Consumer Voice for Quality Long-Term Care, pushed back in subsequent remarks.
“I think we do need to look at how the money is currently being spent by long-term care facilities,” she said. Her group encourages auditing before assessing how much additional funding is needed.
GAO recommendations
The GAO made the following recommendations to curb abuse in its report:
• Require that abuse and perpetrator type be submitted by state survey agencies in CMS’s federal databases for deficiency, complaint and facility-reported incident data, and that CMS systematically assess trends in these data.
• Develop and disseminate guidance — including a standardized form — to all state survey agencies on the information nursing homes and covered individuals should include on facility-reported incidents.
• Require state survey agencies to immediately refer complaints and surveys to law enforcement (and, when applicable, to Medicaid Fraud Control Units) if they have a reasonable suspicion that a crime against a resident has occurred when the complaint is received.
• Conduct oversight of state survey agencies to ensure referrals of complaints, surveys and substantiated incidents with reasonable suspicion of a crime are referred to law enforcement (and, when applicable, to MFCUs) in a timely fashion.
• Develop guidance for state survey agencies clarifying that allegations verified by evidence should be substantiated and reported to law enforcement and state registries in cases where citing a federal deficiency may not be appropriate.
• Provide guidance on what information should be contained in the referral of abuse allegations to law enforcement.
Tuesday’s hearing was live-streamed and can be viewed on the committee’s website.




