Many recovering skilled nursing patients can be discharged to home a week or more earlier without compromising their health, researchers said in a Health Affairs study released Monday afternoon.
Report authors note that findings support both a push for more home-based care and that alternative payment efforts looking to limit SNF lengths of stay “are well-founded.”
While the findings point to a likely slide for skilled nursing demand, they also give nursing homes significant direction, researchers said. Operators should begin proving themselves to risk-bearing partners such as accountable care organizations and bundling groups as efficient, desirable providers in order to rise above others in the market.
“The overall demand in the market for facility care is going to fall. The train has left the station and it’s only going to gain speed,” senior study author J. Michael McWilliams, Ph.D., of Harvard Medical School told McKnight’s Long-Term Care News on Monday. “It may not be the most strategic move to resist [the changes].
“There may be a ‘first-mover’ facility advantage to facilities that start to adapt and become more efficient,” he added. “Get in and get a piece of those savings” with risk-bearing partners.
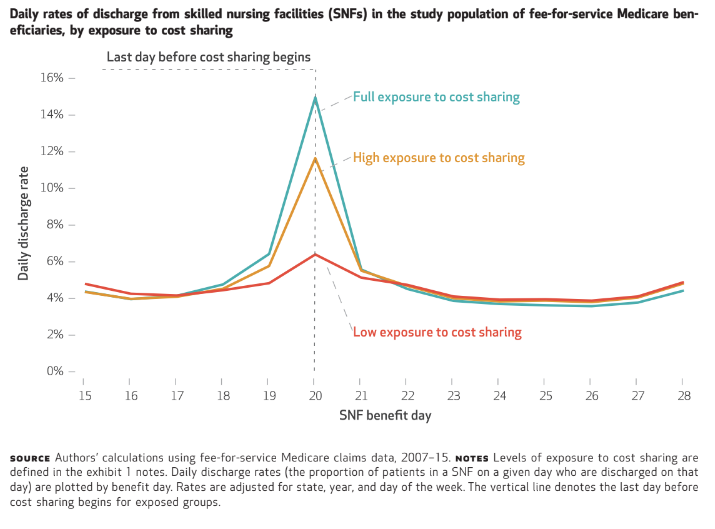
Researchers pivoted their analysis around day 20 of skilled nursing stays for fee-for-service Medicare beneficiaries, after which patient cost-sharing kicks in. Investigators found that patients’ outcomes in days 20 to 28 indicate that earlier discharges actually showed slight reductions in mortality, and “non-significant” rises in falls and all-purpose hospital readmissions.
“Hastening discharge by a week did not affect rehospitalization by day 28 for 98 percent of patients discharged early,” report authors wrote.
“About 10% of patients in a skilled nursing facility could be sent home a week earlier and would be fine,” McWilliams observed. He said earlier studies may have shown savings of just a day or two but now “it appears we can dial it back substantially more.”
Home without help
Lead researcher Brian McGarry, Ph.D., an assistant professor in the Department of Medicine at the University of Rochester (NY) found one discovery particularly intriguing: Some 30% of Day 20 discharges went home and “got no additional services” at all.
“The [reimbursement] policy is very arbitrary and encourages what would appear to be excessively long stays,” he told McKnight’s. Decisions need to be made more often based on clinicians’ criteria, rather than what appears to be financial administration, he said.
He and McWilliams both noted that ACOs and other alternative payment models have already been experimenting with different cost-sharing target days.
“You can imagine, extrapolating from our results, maybe moving up cost-sharing earlier. Instead of day 20, maybe day 10. Interestingly, some Medicare Advantage plans have tried this,” McGarry noted.
He acknowledged that his team’s findings run counter to a similar study about two years ago that found earlier discharges increased the risk of rehospitalizations. He said most analysts agree that the “arbitrary” day 21 onset of patient co-pays, a benefit that goes back to the start of Medicare, “probably is not a great policy.”
“Any time you see this heavy cluster of patients [discharged] on a particular day, it’s evidence these are not strictly clinically evidenced discharges,” McGarry said.
There are no indications, however, that providers have pushed patients out too soon, for there would have been higher rates of reshopsitaliztions, he added.
“What we see is that patients up to day 20 are not incentivized to push back and SNFs also are not pushed by any financial incentives to get those patients home sooner,” he explained. “That doesn’t make for good patient-centered care if you put it in the context of most patients preferring to be home. For the groups we looked at, they can go home sooner and be safe.”
He added that the findings could create great opportunities for home health providers, especially if they evolve. The current system has not “been optimized to deliver more rehab services at home. There’s plenty of innovation that can take place at the home care side.”
The current system may be doing more than artificially depressing home care opportunities.
“We also found a discontinuous increase in hospice use associated with exposure to cost sharing, suggesting that SNFs may delay end-of-life care discussions and referrals to hospice when incentives to lengthen stays go unchecked,” report authors wrote.
‘Waste’ the target
The research team, which also included Harvard Medical School professor of policy David Grabowski, Ph.D., and biostatistician Lin Ding, said it adds to the voices decrying huge amounts of waste in the post-acute care payment system.
“The implications for facilities is that there will be less revenue,” McWilliams said. “It’s just sort of a reality if you’re going to reduce wasteful spending. There will be winners and losers. We’ll see some fall in capacity, which is not necessarily a bad thing. We just need to monitor where that happens. The bigger worry is what the impact would be for long-term patients” whose care is typically subsidized by short-term care funding.
He added that conditions produce “a lot of chances for innovation in the facility setting.” These could include more intensive therapy and care.
“We can expect these efforts to intensify, particularly focused on home-based models with a continued focus on payment reform. Expect risk-bearing providers to be a target for efficiencies. The important thing is we have an ongoing parallel conversation in terms of policy and making sure the patients do well.”
The study examined Medicare claims data of close to 1.5 million SNF stays from 2007 to 2015. Patients were tracked from day 15 through day 28.




