
(Second in a series on providers’ attitudes and concerns about operating conditions in 2024.)
More than half — 55% — of skilled nursing leaders say they would need to hire more agency staff if a proposed federal staffing mandate is enacted.
That’s just one finding from the McKnight’s 2024 Outlook Survey, which reveals operators’ desperation to recruit and retain staff is ratcheting up as a new year begins.
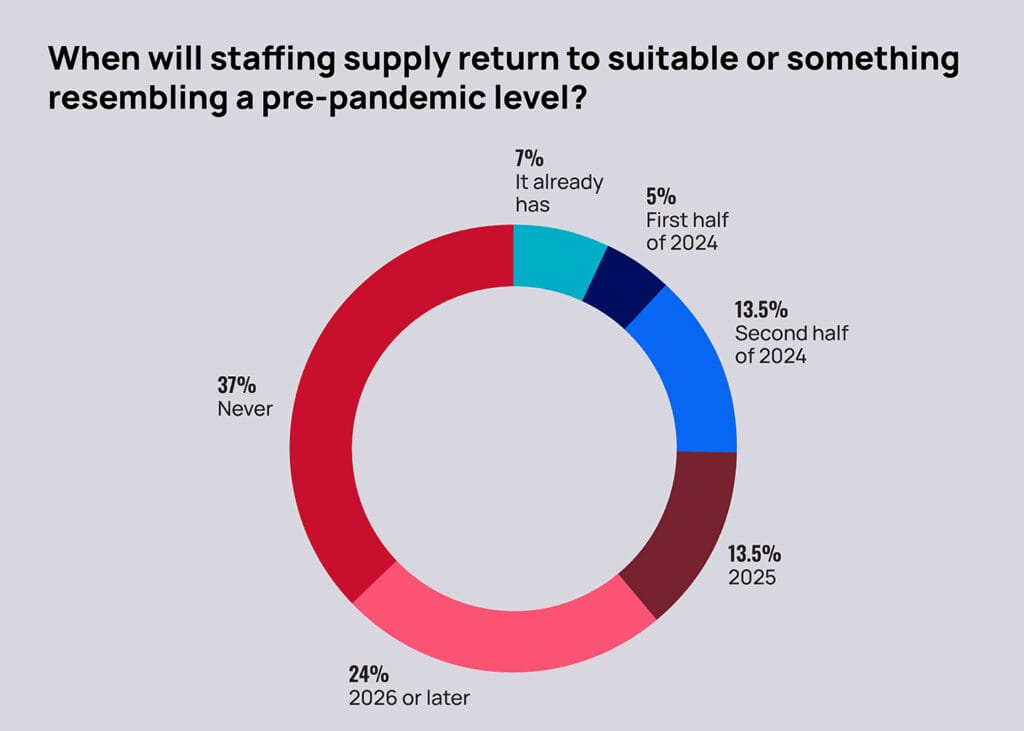
Other findings show that nearly a quarter of respondents (24%) said they don’t expect staffing availability to return to pre-pandemic levels until 2026, and another 37% said that workforce will never return to previous levels. Nearly two-thirds (63%) said they’ve already curtailed admissions because they can’t find enough workers.
That’s the backdrop facing owners, administrators and nursing leaders as they plan for the demands of the year ahead, which could bring a federal staffing rule so stringent that 75% to 80% of all US facilities are projected to need more workers to meet its demands. Added to other significant pressures, hiring challenges could push more providers out of the sector.
“There are these operational issues such as hiring more agency, but pre-mandate, we’re seeing people downsize nursing beds and closing units,” Lisa McCracken, head of research and research analytics for the National Investment Center for Seniors Housing & Care, told McKnight’s Long-Term Care News Thursday. “This is one more pressure shaping how the industry is growing, and shrinking, quite frankly, and it’s all on top of this growing demand and need.”
Skilled nursing occupancy topped 82% in August for the first time since April 2020, according to the latest available NIC Map Vision statistics. In fact, fears about hiring additional staff come even as providers seem remarkably optimistic about census.
Just 8% of respondents (and 5% of administrators) predicted their census would decrease in 2024. Nearly 50% expected it would increase, despite others issuing dire warnings about potential service cut-offs if handed a mandate. About 31% of respondents said they had already returned to pre-pandemic census levels, with another 34% projecting full recovery some time this year.
Nearly four years since the start of the pandemic and its devastating census implications, providers are now having a harder time finding staff than they are landing patient referrals. Most indicate that a staffing mandate would deepen that pain.
“We know that people are living longer and they’re needing that support and whether it’s a short-stay rehab piece in the nursing home or it’s a longer-term safety net and long-term housing option, the need’s there,” McCracken said. “I think what we’re going to be challenged with is, how and where are we going to provide those services? And what is it going to look like? I think that the staffing mandate, while it’s well-intentioned, I don’t know that that’s the solution to some of the challenges the federal government is observing in our space. I worry about the trickle down [effects] of it.”
Agency help unavoidable?
The 2024 McKnight’s Outlook survey shows the staffing crisis’ outsized influence on everything from census to hiring to potential sales. It drew 350 responses from skilled nursing owners, administrators, nurse leaders and other key professionals. It was administered online Dec. 1 through Dec. 28.
Asked whether they’d use more, less or the same amount of agency staffing in 2024 versus 2023, respondents were evenly split, with about one-quarter choosing each option. The other quarter flatly said they don’t, and won’t, use temporary staff at all.
But pressed on how they’d cope with a finalized staffing rule, 55% said they’d have to hire more agency nurses, with that figure registering 60% among administrators. It might be the only way to fill critical slots in coming months.
That’s a reality facing many providers in Maine, explained Angela Cole Westhoff, president and CEO of the Maine Health Care Association. The state has lost more than 20 nursing homes in the last 10 years, a process that has sped up since COVID and the ongoing labor shortage it precipitated.
According to her own December member survey, Westhoff told McKnight’s a “staggering” 86% of Maine long-term care facilities are grappling with a staffing shortage and 60% of those had turned to agency staffing to address critical vacancies.
“Despite use of temporary agencies, many facilities still struggle with staffing and as a result, have either closed to new admissions or taken beds offline, which further decreases access to long-term care,” she said. “Despite all efforts to hire additional staff, the fundamental challenge lies in the scarcity of available workers. The pressing reality is that an unfunded staffing mandate will not fix these challenges.”
Without agency, providers asked to ramp up hourly coverage and at least triple their RN shifts under a federal staffing mandate may be forced to implement more overtime or layer more duties onto existing workers, especially those in administrative roles. That creates added stress on the retention side, too.
Cutting back and finding a way
Agency might be a key strategy for the 45% of survey takers who said they’d “find a way to comply” with the mandate, but another 17% said they’d consider converting beds to a different license type when confronted with a mandate.
Still another 31% predicted they’d need to restrict units or wings due to the mandate. More generally speaking, regardless of a mandate, 51% of respondents said they could foresee having to restrict admission in 2024 “due to staffing or other COVID-related challenges.”
That’s up slightly from the 2023 Outlook survey, when just under 50% of providers told McKnight’s they would have to close in part or in full if federal regulators adopted a 4.1-hour nurse staffing mandate in 2023. That survey was conducted months before the Centers for Medicare & Medicaid Services unveiled its formal proposal, which eschews an overall hourly requirement for individual RN and CNA standards, 24/7 RN coverage and lengthy new facility assessment requirements to account for patient needs.
Without a doubt, a lack of staff contributed to ongoing closures and admissions limitations throughout 2023. The share of survey respondents who said they “curtailed admissions” in 2023 was at 63%, reinforcing reports from a series of state associations that sounded the alarm on growing access issues. Still, that was down from 69% and 73% of providers reporting partial closures in 2023 and 2022, respectively.
In its own commissioned analysis in late 2023, the American Health Care Association found the mandate could displace nearly 300,000 residents if facilities choose to close rather than face stiff penalties for non-compliance.
“Nursing homes that are unable to meet the requirement because they can’t hire the number of necessary RNs and nurse aides will have to limit their admissions or close altogether, further limiting access to care for vulnerable seniors,” the association said.
Providers of all sizes worried
“Staffing continues to be the biggest concern,’ said Amy Stewart, chief nursing officer of the American Association of Post-Acute Care Nursing (AAPACN). “There is a smaller pool of nurses since COVID. Nurses also have more opportunities than working the floor.”
For new nurse graduates, stereotypes about skilled nursing have continued to make it a second choice behind settings where they think they’ll have more opportunities or be able to practice more advanced skills, experts told McKnight’s. Others that used to consider RN careers are following the trend of becoming nurse practitioners, a concern underscored by a 2023 report that found some 900,000 RNs would leave the workforce by 2027.
Still others are simply struggling to gain entry to a convenient and affordable training program, with faculty recruitment issues limiting enrollment and further reducing the job pool, Stewart noted. In many places, there are willing students but not enough instructors.
All of that is frightening to providers, large and small.
“There simply aren’t enough RNs available,” said Nate Schema, president and CEO of the Good Samaritan Society. “It doesn’t add up to think that RNs are going to magically appear now that we have a mandate in place. It simply would create an untenable situation if that mandate was to go through in its current form.”
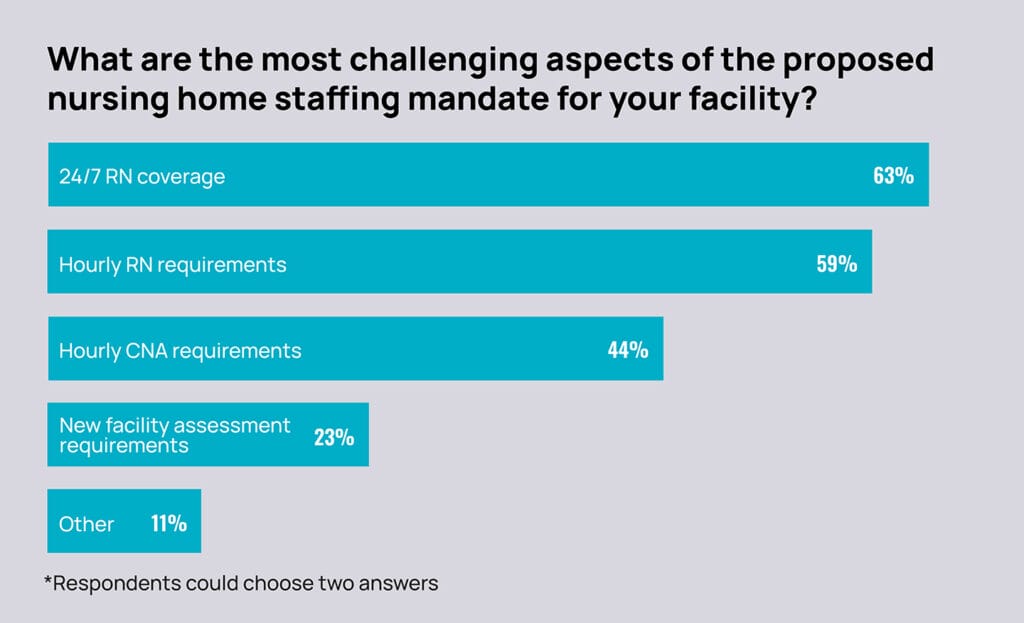
Like most Outlook survey takers (63%), Schema told McKnight’s he would rank the 24/7 RN rule a top mandate concern, followed by the hourly requirement for RNs (which 59% chose in the survey). About 44% of survey-takers ranked hourly requirements for CNAs as a top concern, followed by 23% citing additional facility assessment requirements. Another 11% picked “other” concerns, such as what to do with licensed practical nurses, their clinical mainstay. (Each respondent could choose two answers.)
When asked to rank changes that would make the staffing rule more palatable, providers seemed resigned to the fact that a final rule would not be derailed. Respondents chose inclusion of LPNs in RN time requirements (59%); allowing RNs in administrative roles to count toward hourly stipulations (56%); and providing more funding (52%), respectively. as their top three desired changes. Another one-third said they preferred a “complete withdrawal” by the Centers for Medicare & Medicaid Services, which is currently reviewing nearly 50,000 stakeholder comments on its proposal.




