Nursing home residents could be just a little more than two weeks away from receiving the first doses of a COVID-19 vaccine, according to federal health officials.
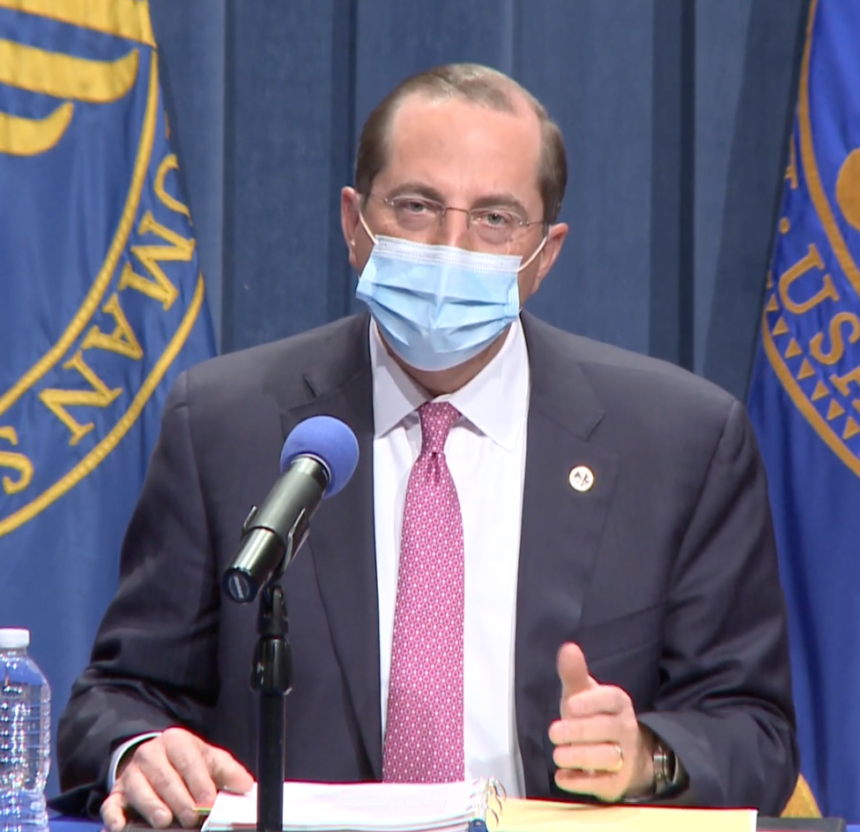
The Food and Drug Administration’s vaccine advisory committee is set to discuss Pfizer’s emergency use authorization (EUA) request for its COVID-19 vaccine on Dec. 10. The federal government could be distributing a vaccine two days after that meeting “if all goes well,” Health and Human Services Secretary Alex Azar said Tuesday morning.
“As all of these pieces come together, we want to try to give Americans the best sense of when our most vulnerable will start receiving vaccines,” Azar said during a briefing. “We believe we can distribute vaccines to all 64 jurisdictions within 24 hours of FDA authorization.
“Then, we hope administration can begin as soon as the product arrives. One of the private sector partners we’ve enlisted, CVS Health, has said that they expect to be vaccinating residents in nursing homes, one of the top priority groups, within 48 hours after FDA authorization,” he added.
HHS Assistant Secretary for Health Adm. Brett Giroir, M.D., in a media call later Tuesday stressed the need for infection control measures, such as universal mask wearing, adequate testing and good hygiene, despite potential vaccines being on the horizon.
He added that the best ways to stop outbreaks in nursing homes is through the correct usage of personal protective equipment and good hygiene by staff members, and by limiting community spread.
“We cannot shield our elderly if we don’t wear masks, avoid crowds, avoid travel if you can [and have] good hygiene,” he said.
Giroir also revealed that the U.S. has spent $20 billion for testing and other needs at nursing homes during the pandemic. About 15,200 facilities have received about 5.3 million point-of-care tests, he added. Additionally, 24.4 million BinaxNOW tests have been distributed to nursing homes, assisted living facilities, historically Black colleges and universities, tribes and other disaster relief efforts.
Giroir noted that the BinaxNOW tests have become a favorite among providers following a call with the major nursing home associations last week.
“Literally, the two most common words [during the call] were ‘game-changer’ and ‘godsend’ for the Binax tests that have been there because they have really revolutionized what they can do in a very quick way,” he said.
Some research has found that just 38% of nursing homes haven’t used the point-of-care antigen testing devices that were shipped to facilities starting in September.





