
The challenges faced by nursing homes came into sharper focus Friday, thanks to a deep dive into skilled nursing since 2015 that attached somber numbers to many industry concerns.
Perhaps most striking is that, despite a rapidly aging population in the US, the total numbers of both nursing facilities and residents in those facilities have dropped, according to the KFF study.
In addition, despite the decrease in available homes and residents, however, the average number of nurse hours per resident per day also has dropped. This reflects heightened concerns about care worker retention and the difficulty of meeting current and proposed staffing mandates that typically require a certain level of hours per resident per day be maintained by facilities.
Left unchecked, these trends have troubling implications, Melissa Brown, COO at Gravity Healthcare Consulting told McKnight’s Long-Term Care News Friday.
“This data is no surprise to any of us in the industry but is rather a confirmation of exactly what we are seeing on the ground,” Brown said. “The idea of having to source and pay for … increased staffing without funding is completely ridiculous and will lead to SNFs slashing beds and shuttering across the country. I believe that if major changes are not implemented now, we will see closures of at least 25% to 50% of the current nursing homes in the next five to 10 years.”
SNF ‘closure tsunami’ feared
The number of skilled nursing facilities certified by the Centers for Medicare & Medicaid Services peaked in 2017, but declined by 4% overall between 2015 and 2023 — a net loss of nearly 650 facilities.
“Everyone is talking about the silver tsunami, but no one seems to be talking about the coming SNF closure tsunami,” Brown told McKnight’s. “We are barely scratching the surface of SNF closures, but I can clearly see the SNF closure tsunami on the horizon, and the KFF report supports that.”
Meanwhile, the total number of nursing home residents dropped even more sharply, by 12%, during the same period. Changing trends in where older Americans choose to receive care are a major factor in this decline, the KFF report noted.
“Decreasing resident counts reflect longer-term trends as people increasingly opt to receive care in home and community-based settings over institutional settings,” they explained.
They also noted the tragic impacts of the COVID-19 pandemic on the residents of nursing homes. In fact, despite the notable overall decline since 2015, the number of nursing home residents are again on the rise from their lowest point of 1.1 million in 2021 amid the height of the pandemic. The total now stands at 1.2 million after increasing each of the last two years.
The 2021 low point in the total number of residents coincided with the highest point for care hours per resident day in the last six years. Since 2021, that number has declined as the resident population began to rebound. It now sits at 3.77, a 9% decline since 2015.
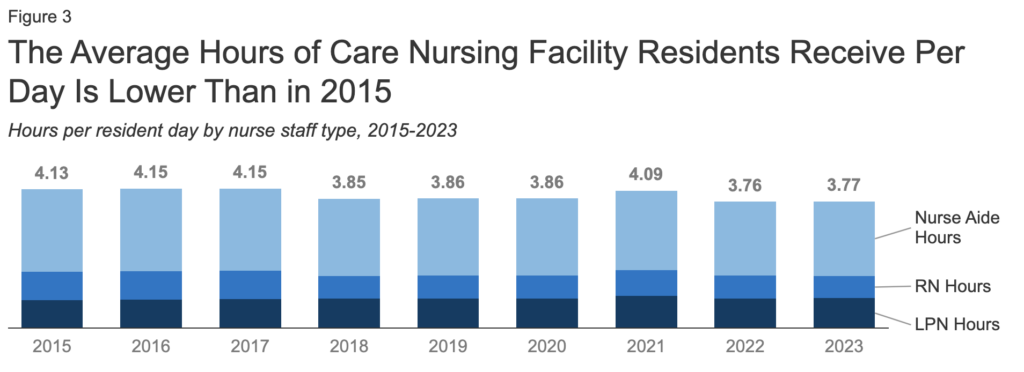
“The relatively higher staffing hours in 2021 reflected the fact that the number of residents declined more quickly than the number of staff hours did between 2020 and 2021,” the report’s authors wrote. “Lower staffing levels in the last several years align with data … showing that the number of workers employed at long-term care facilities continues to remain below pre-pandemic levels.”
Staffing problems remain at the front of sector concerns going into 2024. The data on the average number of deficiencies per facility may only add fuel to that fire.
That number now stands at 8.9 and has steadily increased since a low point of 6.8 at the report’s 2015 start date. The authors noted that studies have shown facilities with better staffing typically have fewer deficiencies, and so this broad increase in deficiencies may be related to staffing woes.
Ever-increasing staffing demands may lead to further negative effects in the future, according to brown.





