
Rising inflation and increased labor costs are multiplying the risk of closure for skilled nursing facilities across the country, according to a new analysis released Wednesday by CliftonLarsenAllen and the American Health Care Association.
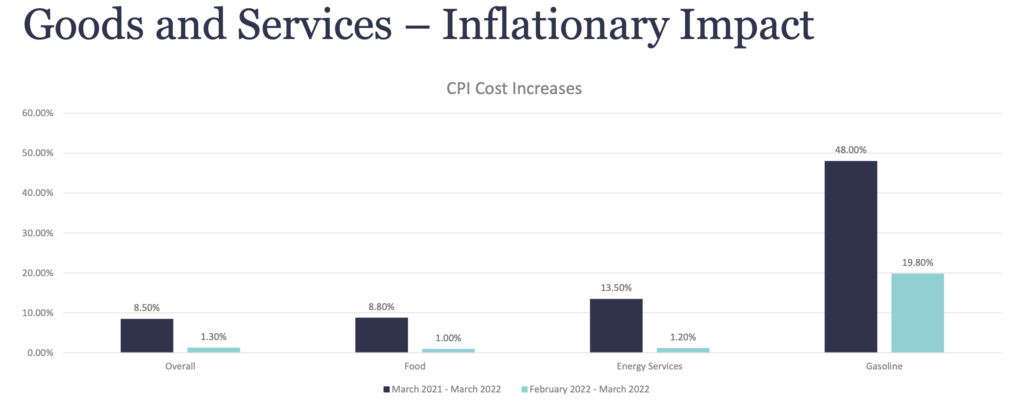
The findings from CLA show that general inflation for nursing home goods and services increased 8.5% between March 2021 and March 2022. It leaped 1.3% just between February and March earlier this year.
Food costs rose 8.8% between March 2021 and March 2022. During the same period, gas prices soared 48%. The jump was 19.8% from February to March earlier this year.
Economists expect even more increases through the end of the year, and possibly into 2023, which is more bad news for providers. Nursing homes rely almost entirely on fixed-rate government payments. “Increasing costs will put more nursing homes at financial risk,” AHCA noted.
CLA used key driver assumptions such as occupancy, reimbursement changes and inflation to construct more than 12,800 site-level simulations to assess SNFs’ 2022 outlook.
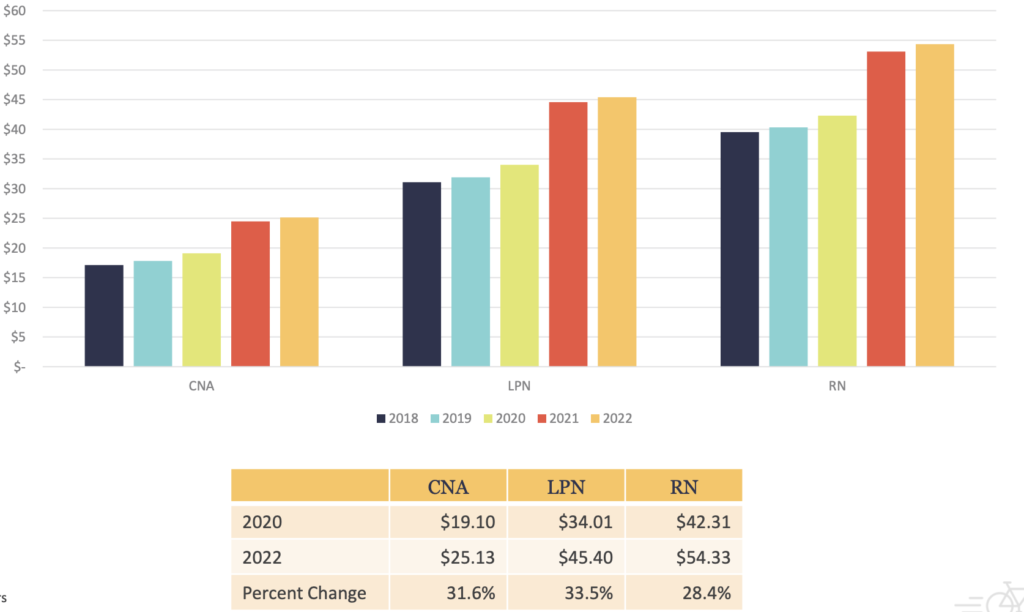
The firm’s report included survey findings on nursing costs from more than 330 facilities across 24 states.
CLA said that the number of residents living in facilities at financial risk of closing will triple — to 47% (417,000 residents). By comparison, just 16% of nursing home residents lived in at-risk facilities in 2019.
Data also showed that hourly nurse pay rates jumped at least 28% in each of three categories. Certified nursing assistants’ average hour pay increased 32% from 2020 to 2022 (from $19.10 to $25.13). The rise for LPNs was 33.5% ($34.01 to $45.40), while registered nurses saw their average pay bounce 28.4%, from $42.21 to 54.33.
CLA principal Deb Emerson said the report helps providers understand the local, real-world impact related to the ongoing economic challenges facing nursing homes.
“Erosion in financial performance creates the potential for a greater negative impact on hundreds of thousands of residents, especially racial and ethnic minority populations,” Emerson said. “The entire industry will be faced with the difficult task of balancing available capacity while maintaining health equity and serving the health needs of nursing home residents.”





