House Republicans Wednesday took aim at the Biden administration’s proposed federal staffing rule, saying it would threaten access to and disrupt care in nursing homes.
The criticism was echoed by several witnesses representing a range of long-term care perspectives during a hearing on two proposed regulations and their impacts on workforce and access to long-term care services and supports.
Republicans also objected to a proposed home- and community-based services rule that would force 80% of payments to be spent on direct care, a change that could devastate state Medicaid systems that also would be tasked with paying skilled nursing providers for increased staffing.
“While well-intentioned, these rules are misguided and will ultimately threaten to undermine access to vital services that our most vulnerable rely upon,” said Rep. Brett Guthrie (R-KY), chair of the House Committee on Energy and Commerce Subcommittee on Health. “We’re at a critical juncture for our long-term care system. Since the start of the pandemic, we’ve lost hundreds of thousands of workers from nursing homes, as well as home- and community-based services, while more Americans continue to age and need more long-term care.
“More needs to be done. However, instead of partnering with Congress, the Biden administration is embracing central planning, claiming their proposal will lead to more workers being hired and help ensure safety,” added Guthrie. “Unfortunately, this is far from reality. These one-size-fits-all, Washington-knows-best approaches will impose unfunded mandates on states and providers, while reducing access to vital services without addressing the root cause of the problem.”
Guthrie last week joined nearly 100 House members from both parties in penning a letter to Health and Human Services (HHS) Secretary Xavier Becerra. It raised major concerns about the staffing rule proposed in September. Subcommittee member Rep. Greg Pence (R-IN) has also cosponsored a bill to block the proposal, which had 10 total cosponsors as of Tuesday.
Republican subcommittee members stacked Wednesday’s panel with witnesses who expressed dismay, fear and continued disbelief at the staffing proposal’s timing.
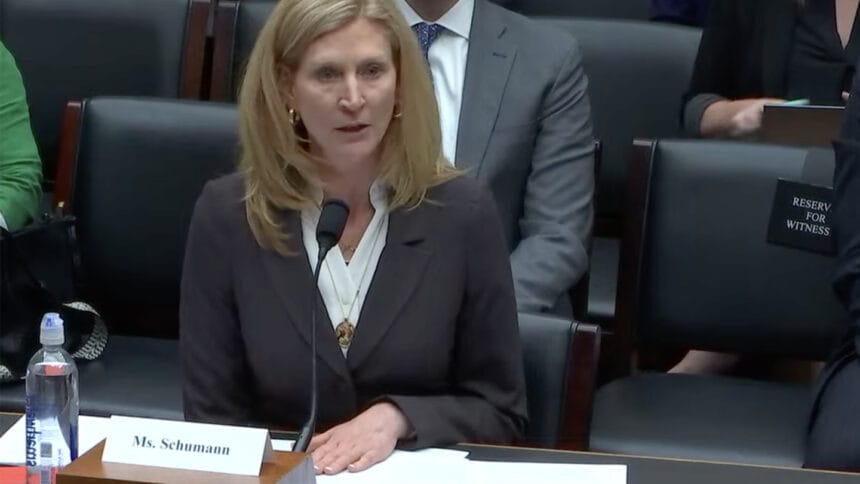
Among them was Sarah Schumann (pictured above), vice president of operations at Colorado-based Brookside Inn and Brookside Rehabilitation, who described her family-owned facility’s efforts to improve staff retention and recruitment.
She called the combination of the workforce crisis and the looming mandate “terrifying and heartbreaking,” noting that the rule’s interpretation and potential penalties could force her to close her majority-Medicaid facility.
Not owned by Wall Street
Despite increasing salaries by an average of 40%, with CNAs now being paid $23 an hour to start, Schumann said she still struggles with hiring. She also has greatly improved benefits, covering healthcare for employees and their families as well as offering 3.5 weeks of paid vacation. And even with those industry-leading standards, she said, she cannot find enough staff “simply because the number of qualified caregivers that we need are not there.”
Colorado, she noted, has waived its own requirement for round-the-clock registered nurse staffing in nursing homes, acknowledging providers’ inability to hire enough RNs. The federal mandate would layer that requirement over daily per-patient care requirements for RNs and certified nursing assistants. Schumann predicted that would lead to additional dependence on agency staff — a shift that would affect care and prove “financially unsustainable.”
She questioned whether the administration is seeing the unintended consequence the staffing mandate would trigger in facilities that serve a disproportionate share of underserved seniors, or those located in underserved communities.
“Like most of the profession, Wall Street does not own my company,” said Schumann, who started in the business as a chaplain and CNA. “We serve residents on Medicaid, and we do not have the resources to fund this unfunded mandate. … We cannot be expected to just magically grow new caregivers.”
Especially concerning to Patti Killingsworth, former Chief of LTSS for TennCare and chief strategy officer for CareBridge Health, is the idea that a rule limiting HCBS spending and a rule driving more required SNF spending would overlap.
That could hit state budgets especially hard, just as the demographic demand for long-term care in a facility or at home increases. That, she said, could lead to reduced services in both sectors.
Opposing voices heard
The hearing, held immediately following a vote to elect a new Speaker of the House after nearly three weeks without one, was unusually well attended. Lawmakers’ questions and comments stretched the conversation to three full hours.
Despite concerns expressed by most witnesses about the consequences of a mandate, several Democrat subcommittee members hewed to the party line, accusing sector advocates of making the issue all about money.

“The Biden administration has proposed what they view as a solution to the lack of staff providing care in nursing homes. Red light and siren: Hire more people. It’s as simple as that,” said ranking member Rep. Anna Eshoo (left, D-CA).
“We’ve all, I think, been in a hospital or a healthcare setting where there’s a button, and when we press that button, we want someone to come to us,” she added. “Does it cost something? Of course it does. Of course it does. But if no one comes when you press the button, things go downhill from there.”
Witnesses including a CNA from Bellingham, WA, and Lori Smetanka of the National Consumer Voice for Quality Long-Term Care, underscored the need to move the needle on both recruitment and retention. They focused their comments on needing a mandate to push higher staffing levels, a move they said would result in more attractive jobs and contribute to lower turnover.
“If you can’t keep staff, that’s going to be a problem when you’re needing to continue to fill positions with new people,” Smetanka said. “A really important part of this issue is talking about how to reduce the turnover, how we need to improve job quality conditions for workers so that they’re wanting to stay in these facilities and stay in this field.”
Clif Porter, senior vice president of government relations for AHCA/NCAL, said in a statement that he hoped providers would follow an example set in Schumann’s testimony and ask the White House and their Representatives to work together “on more meaningful and comprehensive policies that will actually help long-term care facilities recruit workers as well as build a strong pipeline of caregivers.”
For more coverage from this hearing and its focus on proposed spending rules for home and community-based services, see McKnight’s Home Care.



