
Nursing home workers’ COVID-19 vaccination rates increased by 25 percentage points in the months after the federal government mandated all healthcare workers receive shots, according to an analysis by the Kaiser Family Foundation.
Nationally, rates jumped from 63% to 88% between the Biden’s administration announcement of a vaccine requirement in August 2021 and the mandate’s Supreme Court-backed enactment this March. That’s a net 40% increase from the 63% starting point.
“While a number of factors may have been at work, it appears that the mandate contributed to the increases in staff vaccination rates,” KFF researchers reported Monday
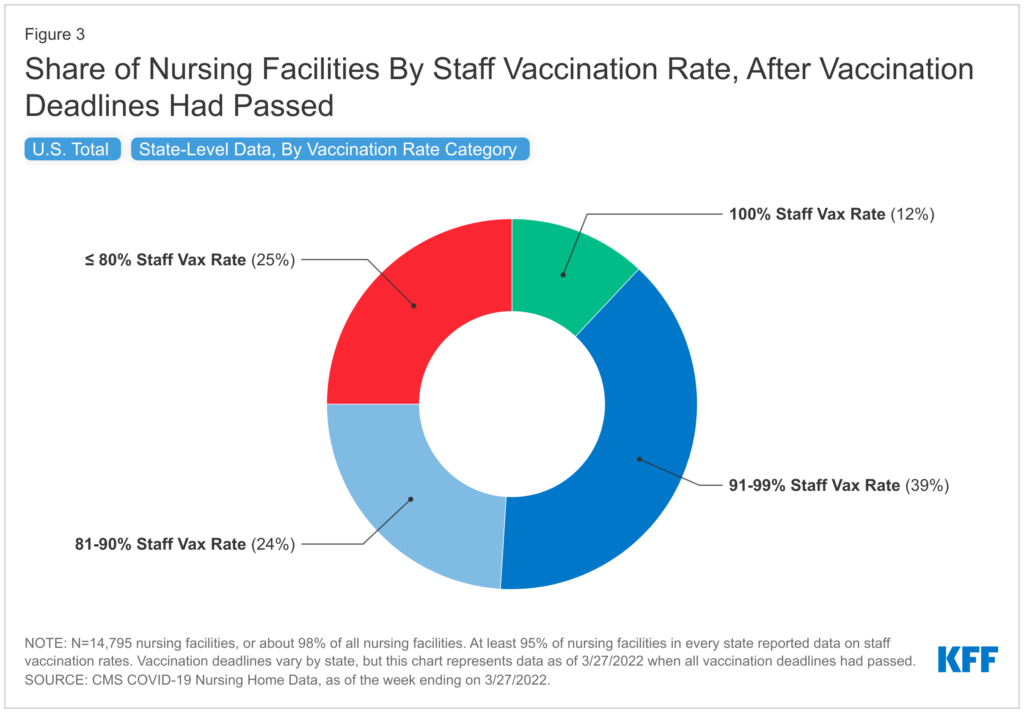
They reviewed publicly available nursing home-level data covering about 97% of all nursing homes in the U.S. to find that, as of March:
- 12% of nursing homes reported 100% of workers fully vaccinated
- 39% had a better than 90% vaccination rate
- 49% had fewer than 90% fully vaccinated
While many nursing home operators and some state officials argued that mandates would push workers out the door, the KFF analysis refutes that thinking.
“Data suggest that the vaccine mandate has not exacerbated staffing shortages to the extent initially hypothesized since shortages have actually fallen nationally since January 2022,” analysts wrote. “There are likely a multitude of factors that impact staffing shortages beyond the vaccine mandate,” including local economies and labor markets.
KFF found that 28% of U.S. nursing homes reported staffing shortages in March, which was actually down slightly from a January peak. At that time, in the midst of the first omicron wave, about one in three nursing homes reported a shortage.
One weakness underscored by the KFF analysis was the struggle to get workers boosted.
As of March 2022, the national booster rate for nursing facility staff was 44%, ranging from 93% in Massachusetts to 24% in Florida, Missouri and Mississippi.
While the federal mandate does not explicitly require booster shots, Conneciticut, Massachusetts, New Jersey, New York and California did pass state laws requiring them. Those states reported gains of more than 30 percentage points in booster coverage between January and March.
Nationally, about one-third of facilities reported booster rates among nursing facility staff higher than 50%, with another one-third reporting booster rates under 25%.
Some providers have said that the government’s failure to coordinate booster delivery to nursing homes has limited uptake of third and fourth doses, especially among workers who may not be present for smaller clinics.
And a looming funding crisis could make efforts to further coverage even more difficult. Politico reported last week that administration officials are starting to consider hard choices as Congress remains stalled on passive massive new COVID funding.
“Inaction in Congress is already forcing difficult and unnecessary compromises that have dire consequences for the American people,” a White House spokesperson told the news organization, warning of “even more difficult tradeoffs.”
Politico said funding delays or inadequacy could force the government to put off buying new vaccines better matched to omicron variants and limit future shots to only the “highest-risk populations.” It’s unclear if that would include both long-term residents and staff.




