The COVID-19 mitigation strategies of social distancing, face coverings and handwashing not only will help to curb the spread of the coronavirus, they will help to lessen the severity of the upcoming flu season, the head of the Centers for Disease Control and Prevention said.
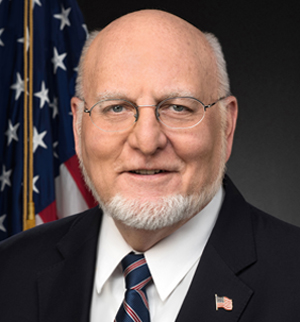
“If we all did that for four, six, eight, 10, 12 weeks, the COVID outbreak in the United States would really be brought to its knees,” Robert Redfield, M.D., CDC director told McKnight’s Thursday. “If we continue to do that in the fall … we’ll have a really mild flu season.”
Redfield drew a comparison to Australia, whose seasons are off-cycle from the United States and currently has little flu because of the nation’s adherence to prevention strategies. Such tactics “will not only affect COVID but other respiratory viruses,” he said.
By contrast, he posed that if the American public does not practice these measures, “we could end up with two serious pathogens coming through at the same time and, as a consequence, have a very difficult time in terms of our response,” he said, with “the pathogens putting stress on our healthcare system.”
Worker testing, flu shots
Redfield also stressed the importance of weekly COVID-19 testing and flu shots for nursing home workers. Given the strong asymptomatic aspect of COVID-19, unlike the flu, testing is critical to stopping the spread from workers to residents.
“The only way you’re going to know is to start an aggressive surveillance program,” he said.
He pointed out that there is a new recurrence of substantial transmission of the coronavirus in nursing homes throughout the United States.
“This virus is continuing to be reintroduced to nursing homes and we need to shut that down,” he said.
Flu vaccination rates among long-term care workers continue to be a problem, he said. While vaccination rates are strong among healthcare workers in hospitals, they lag among nursing home workers at under 70%, Redfield noted. As a result, nursing home facilities need to make receiving the flu vaccine mandatory, he said.
“I would encourage the owners of these facilities to make this a requirement, like it [had] been made for me to be able to work in my hospital when I practiced medicine,” Redfield said.
Data collection
The CDC’s National Healthcare Safety Network (NHSN), which is collecting information from nursing homes on COVID-19 cases, is a “critical surveillance system,” Redfield said. It recently was developed to gather data on antibacterial and antifungal resistance and is now being used in the fight against the coronavirus.
NHSN is an important tool to understand COVID-19 and “begin to have real-time data on the parameters of COVID infection in long-term care facilities, particularly as new therapeutics are developed which may have unique benefits,” he said.
The Trump administration now is requiring states to provide data from hospitals to the Department of Health and Human Services and not the CDC, which was the previous protocol.
“This streamlining will allow the NHSN to increase its focus on another critical area for COVID-19, the nursing home and long-term care facility reporting needs — which, as we know, is also an absolutely central element of our pandemic response,” he said during remarks to the media on Wednesday.





