Now that some nursing home operators have begun receiving point-of-care antigen testing devices from the federal government, the question remains where they will obtain the supplies needed to comply with long-term testing requirements — and how they will pay.

All U.S. nursing homes are slated to receive the diagnostic equipment, starting with those in COVID-19 hotspot counties. In states with a 5% or greater positivity rate, operators are expected to test all nursing home staff each week, the Centers for Medicare & Medicaid has said.
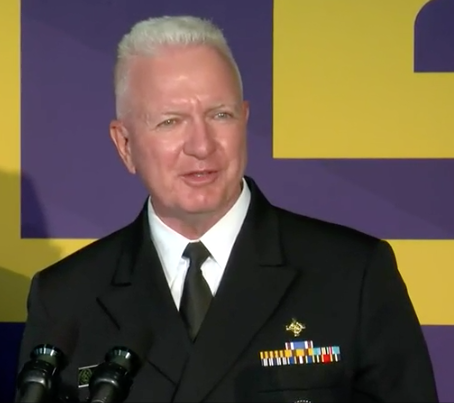
But the government isn’t planning to send more than the initial rounds of test kits. Instead, facility operators are responsible for procuring additional tests directly from manufacturers or medical device distributors, said Adm. Brett Giroir, assistant secretary of the Department of Health and Human Services, during a call with operators at the time of the announcement.
CMS has categorized the expected single-shipment deliveries by facility size:
- Small facilities: 150 tests, 1 instrument
- Small-to-medium facilities: 240-250 tests,* 1 instrument
- Medium facilities: 325-330 tests,* 1 instrument
- Large facilities: 600 tests, 1 instrument
- Major outlier facilities: 900+ tests, 2 instruments
*Test kit sizes vary by device manufacturer
Industry advocate LeadingAge has estimated that a “conservative” weekly cost for antigen testing, staff time, and retesting negative results as recommended by the Food and Drug Administration could run from $19,265 to $37,590 per facility, based on number of employees. “This estimate does not include the additional [personal protective equipment] needed to conduct tests,” the organization added. Adm. Giroir has said that repeat testing may not be necessary in all cases.
Meanwhile, federal health officials have said generally that eldercare facilities can pay for ongoing infection control measures from their portion of the $5 billion Provider Relief Fund authorized by the Coronavirus Aid, Relief, and Economic Security (CARES) Act. The details regarding test kits remain uncertain, however.
“I think the biggest fear is that the instruments may be delivered but it won’t do any good, if you don’t have the test kits,” George Linial, president of LeadingAge of Texas, told the Associated Press.
“Part of the problem is resources and a lack of clarity about who pays for this in the future.” said Tamara Konetzka, Ph.D., a professor at the University of Chicago, told the news outlet. “Doing one round of testing doesn’t really solve the problem in a pandemic that could last months or years.”
It may be awhile before all facilities receive the testing devices. CMS has stated that it expects the rollout could take up to 14 weeks from July 20, based on supply availability. Only “a few dozen” of Texas’s 1,200 nursing homes have received the equipment so far, Linial told the AP.
An updated list of nursing homes eligible to receive devices and related equipment can be found on this CMS data page. Facilities will receive either the Quidel Sofia 2 Instrument or a Becton, Dickinson and Company (BD) Veritor™ Plus System.
To be eligible, nursing homes must have a current CLIA Certificate of Waiver and meet certain epidemiological criteria.




