Plus other industry news:
- Nursing home prescribes hydroxychloroquine to ill residents
- Operator changes policy: Face masks must be worn ‘at all times’ during COVID-19 crisis
- Broad-based testing could prevent ‘heartbreaking’ spread of COVID-19, says operator with experience
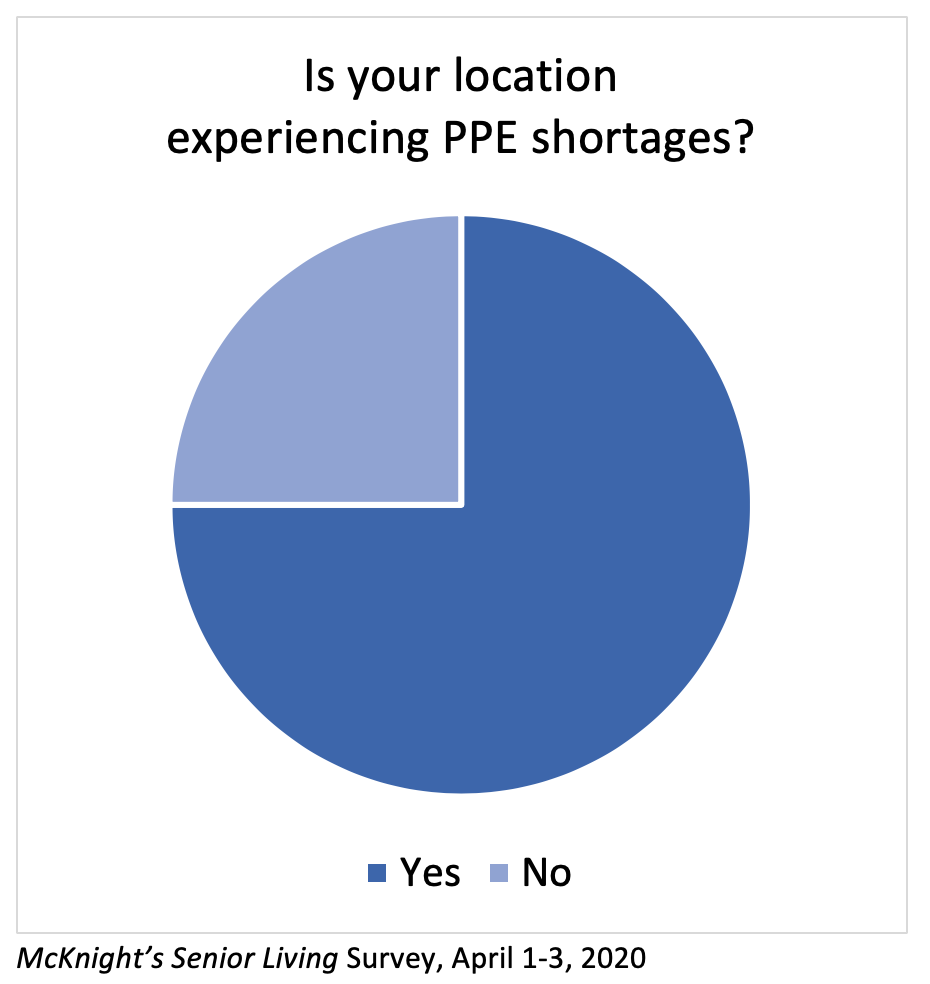
As many areas of the United States anticipate a coming surge in COVID-19 cases, three-fourths of respondents to a new McKnight’s Senior Living editorial survey report shortages of personal protective equipment in their independent living, assisted living, memory care or continuing care retirement communities.
Additionally, 64% of survey participants said their communities are using homemade or improvised PPE or are reusing equipment.
Masks, gowns, gloves and shoe covers are just some of the infection control products that are considered PPE.
McKnight’s Senior Living conducted the survey April 1 to 3 via email; 336 usable responses from administrators, owners, operators, health and wellness leaders, frontline caregivers and others working in senior living were received.
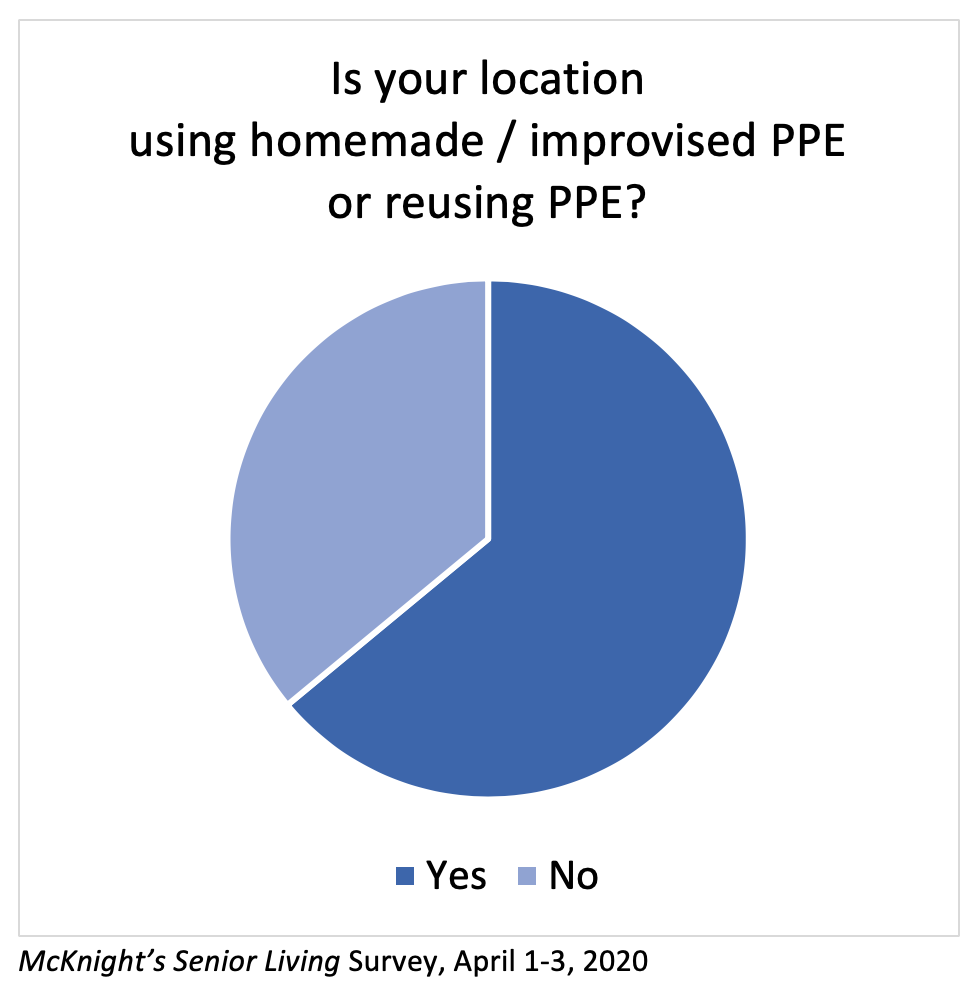
“We are using homemade masks, as we are allotted one box of 50 masks a month. I have 53 employees,” one participant said.
Another respondent cited adequate PPE and hand sanitizer “for now,” but said, “We would like resources for the future, since our vendors may not be able to meet the need.”
“We need gowns, masks and sanitizer within two weeks,” another participant said.
In addition to needing PPE, some communities need guidance on how to store and reuse it, one respondent said. “I hear facilities are storing masks in brown paper bags and others putting them in Ziploc bags. What is the safest way? Where do you keep them?”
77% report no cases yet
Seventy-seven percent of survey-takers said that no cases or presumed cases of COVID-19 had been detected among residents or workers in their communities, but 65% of participants said their communities currently are equipped to care for residents or patients who have the disease.
One respondent even works in a building that has prepared a separate wing with negative air flow for people who test positive for the disease. Another respondent who works in a building getting ready to accept older adults with COVID-19, however, anticipated that some staff members will call off when the sick residents are admitted.
See McKnight’s Senior Living for additional survey results.
In other coronavirus-related news:
Nursing home treats residents with hydroxychloroquine: A Texas nursing home clinician is using the malaria drug hydroxychloroquine to treat more than two dozen residents who have tested positive for the coronavirus, reports the Texas Tribune. The drug’s efficacy has been hotly debated nationwide, with some clinicians urging caution regarding its use in the elderly. The Food and Drug Administration on March 28 issued emergency use authorization for the decades-old drug.
Operator changes policy: Face masks must be worn ‘at all times’ during COVID-19 crisis: All caregivers and providers working in Sanford Health and the Good Samaritan Society facilities must now wear surgical face masks “at all times,” the operator announced in a Monday post. “This proactive action will help minimize virus transmission from people who may carry COVID-19 but aren’t showing symptoms,” said Allison Suttle, M.D., Sanford’s chief medical officer.
Broad-based testing could prevent ‘heartbreaking’ spread of COVID-19, says operator with experience: A top executive at Seattle-based Era Living wants health officials to make COVID-19 testing immediately available for residents and care providers. Nisan Harel, vice president of operations, called for action after one of his communities had prevention success with rapidly deployed testing, reports McKnight’s Senior Living Editor Lois Bowers.
Immune system ‘storm’ may explain why some COVID-19 patients crash: The body’s immune system may overreact to SARS-CoV-2, the virus responsible for COVID-19, physicians tell NPR. This can create what is known as a cytokine storm, leading to a patient’s quick downturn.





