
Every skilled nursing facility in the US will be subject to a five-claim audit starting the week of June 5 as regulators try to better assess and root out improper payments.
The Centers for Medicare & Medicaid Services announced the audits by Medicare Administrative Contractors in early May, later removing a related memo from public view. But several experts have said the reviews still will take place on a rolling basis, with MAC in every region required to pull five Medicare Part A claims from every facility they cover and review them for potential errors.
The results will lead to basic education, adjustment to prepayment claims and more in-depth, one-on-on-one education for providers who have errors on more than one-fifth of their claims. The effort follows a Health and Human Services report that found skilled nursing facilities had the highest rate of improper payments, with nearly a quarter of those tied to insufficient documentation.
“We haven’t seen anything like this in the recent past, at least not in the last 10 years,” said Stacy Baker, OTR/L, RAC-CT, director of audit services for Proactive LTC Consulting. “But it’s no surprise to see this sector-wide probe and educate. Looking back on Medicare FFS improper payment data, we’ve never seen SNF improper payment rates this high, and nearly doubling since the 2021 report.”
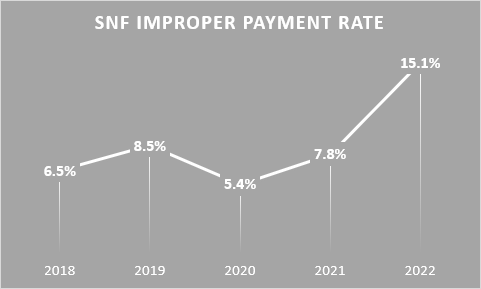
That rate stood at 15.1% in 2022, almost double the 7.79% rate in 2021. A CMS report blamed missing case-mix group component documentation. Baker billed the new initiative as an attempt to improve poor billing practices that emerged with the implementation of the Patient Driven Payment Model.
But the improper payments can’t be attributed to PDPM alone, said Alicia Cantinieri BSN, vice president of MDS policy and education for Zimmet Healthcare Services.
“That’s probably not the whole reason,” she said on a webinar earlier this month.
She noted that risk areas that could move providers to the front of the audit process include past performance, such as a history of additional documentation requests (or ADR); frequent errors in Section GG, which sets payment rates for physical therapy, occupational and nursing groups; diagnoses without medical record to support MDS inclusion; and even illegible RN signatures.
The reviews will be conducted on a prepayment basis unless the provider requests post-payment review due to a financial burden. To prepare, Baker said, providers should review their triple-check process to ensure a strong clean claims process is in place.
“Keep in mind, there’s lots of low-hanging fruit for payment error aside from PDPM accuracy, such as but not limited to, compliant SNF Certs and Recerts and physician oversight regs,” Baker added. “These components should be included in the Triple Check process as well.”
The CMG for each HIPPS code also must be clearly supported to validate the claim, she added.
While this audit won’t be as intrusive as some, providers still should take steps to prepare.
“The MACs are going to complete one round of probe and educate for every provider, instead of that usual potential three rounds, as per their traditional TPE program, that target probe and educate [and] education is going to be based on any identified errors,” Cantinieri explained.
Baker said it’s a good idea for providers to start analyzing data and conducting internal audits. Some EMR softwares offer capability of seeing PDPM data elements as compared to peers, and Zimmet is offering a service that allows providers to see their risk score.
Providers can also review their Program for Evaluating Payment Patterns Electronic Report (PEPPER), to see any “outlier billing patterns,” Baker added.
In addition. Baker offered these tips for an effective ADR response:
- Develop a process and team now. Assign responsibilities for tasks such as, but not limited to: identifying ADR requests, ensuring timely response to deadlines are met, pulling together medical records and documents required to support the HIPPS code, and reviewing the packet for completeness.
- Organize documentation to make the contractor’s review easy, labeling critical sections such as physician orders, MDS assessments, Section GG documentation and more.
- Allow sufficient time for staff with clinical and MDS coding expertise to review the claim and documentation for accuracy and to write a defensive brief if possible.
- Maintain a copy of the entire packet provided to the MAC in case of appeals.
- Document and maintain records/receipts of timely submission of the ADR following contractor guidelines.




