Nursing homes will be required to deliver 3.48 hours of daily direct care per patient under a final staffing mandate issued this morning.
A White House statement on the rule today said that 3.0 hours must be split between registered nurses at 0.55 hours and 2.45 hours for certified nurse aides. The remaining time was not immediately defined by the White House release, and the full rule text was not available.
“When facilities are understaffed, residents may go without basic necessities like baths, trips to the bathroom, and meals – and it is less safe when residents have a medical emergency,” the White House said in a statement. “Understaffing can also have a disproportionate impact on women and people of color who make up a large proportion of the nursing home workforce because, without sufficient support, these dedicated workers can’t provide the care they know the residents deserve.”
The rule also preserves a requirement proposed in September that requires facilities to have an RN onsite 24 hours a day, seven days a week.
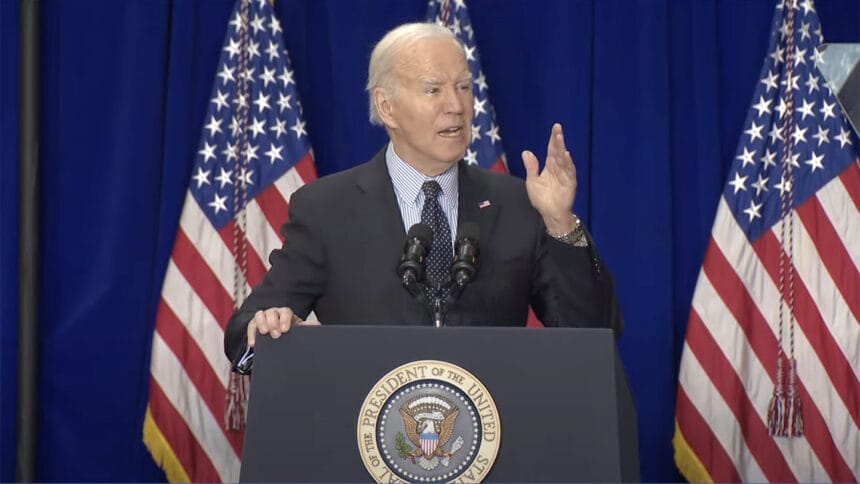
In his 2022 State of the Union address, President Biden pledged that he would “protect seniors’ lives and life savings by cracking down on nursing homes that commit fraud, endanger patient safety, or prescribe drugs they don’t need.”
Nursing home provider organizations and leaders of facilities across the country have decried the rule’s timing, given an ongoing and historic loss of workers that started during the pandemic.
“It is unconscionable that the Administration is finalizing this rule given our nation’s changing demographics and growing caregiver shortage,” Mark Parkinson, president and CEO of the American Health Care Association/National Center for Assisted Living said in a statement Monday morning. “Issuing a final rule that demands hundreds of thousands of additional caregivers when there’s a nationwide shortfall of nurses just creates an impossible task for providers. This unfunded mandate doesn’t magically solve the nursing crisis.
“The Administration has gone ever farther than originally proposed, making these requirements even more out of touch and out of reach,” he added. “At the end of the day, the agency is overstepping with a one-size-fits-all enforcement approach that is deeply flawed.”
While CMS in its proposed rule estimated a cost of $4 billion annually, other industry estimates started at $6.8 billion and have already floated significantly upward due to inflation. The agency had so far offered no funding for its staffing initiative beyond a one-time, $75 million allotment that one CMS leader said this week could be used to market nursing home jobs and create financial incentives to help nurse aides pay for training.
Staffing battle to continue
Today’s final rule is very likely not the final word on nursing home staffing minimums.
Active bills in both houses of Congress could block the rule, and at least one provider group has said it could sue to thwart adoption should the final rule be unworkable.
“This fight is not over,” AHCA’s Parkinson said today. “We will vigorously defend our nursing home members, those they serve, and those they employ. Momentum against the mandates continues to build among both Democrats and Republicans, and we hope to work with lawmakers on more meaningful solutions that would help boost the long term care workforce. For the sake of our nation’s seniors and their caregivers, we must find a better way.”
The initial proposed rule issued Sept. 1 called for all nursing homes to provide round-the-clock registered nurse coverage, as well 2.45 hours per-patient, per-day care by a nurse aide and 0.55 hours of per-patient, per-day care by an RN.
That proposal did not include minimum standards for licensed practice nurses, a detail many providers said would force them to downsize their LPN ranks in favor of hiring more required RNs.
But the agency had also asked for feedback on changing to a 3.48 hourly standard that could include a broader swath of nursing types.
Initially, non-rural nursing homes would have had three years to comply with some elements of the rule, with rural facilities given five years to get up to speed on the hourly rates.
The RN coverage rule, triple the current standard, was proposed to go into effect two years after the rule is finalized for urban providers, with another year granted to rural providers.
The proposed rule did include an option for hardship waivers, an element providers had pleaded for given the sector’s ongoing workforce crisis. In the months following the proposal, however, some providers said the hardship process as designed would require too much work.
The mandated per-day levels are well below the 4.1 cumulative hours per day level that a CMS study recommended in 2001. But even by early CMS estimates, some 75% of nursing homes were predicted to need additional staffing to comply.
Most said they would have the hardest time hiring RNs, who often opt for the higher pay and more flexible work schedules offered in other healthcare settings. Nationally, there is also an ongoing shortage of about 203,000 RNs, an annual discrepancy that is expected to last through at least 2031 according to the federal Bureau of Labor Statistics.
More from White House
The Centers for Medicare & Medicaid Services had not posted any details on the rule as of 10:30 a.m. ET.
The White House, however, said that “limited, temporary exemption”s will be available for both the 24/7 registered nurse requirement and the hourly standards for nursing homes in workforce shortage areas that demonstrate a good faith effort to hire.
“Strong transparency measures will ensure nursing home residents and their families are aware when a nursing home is using an exemption,” the White House added. “This rule will not only benefit residents and their families, it will also ensure that workers aren’t stretched too thin by having inadequate staff on site, which is currently a common reason for worker burnout and turnover. Workers who are on the frontlines interacting with residents and understanding their needs will also be given a voice in developing staffing plans for nursing homes.”
This is a developing news story. Please check back for more.




