As the clock counts down to the release of the Biden administration’s promised nursing home staffing mandate, providers are hoping that a growing chorus of federal lawmakers opposed to the idea will stem the potential harm.
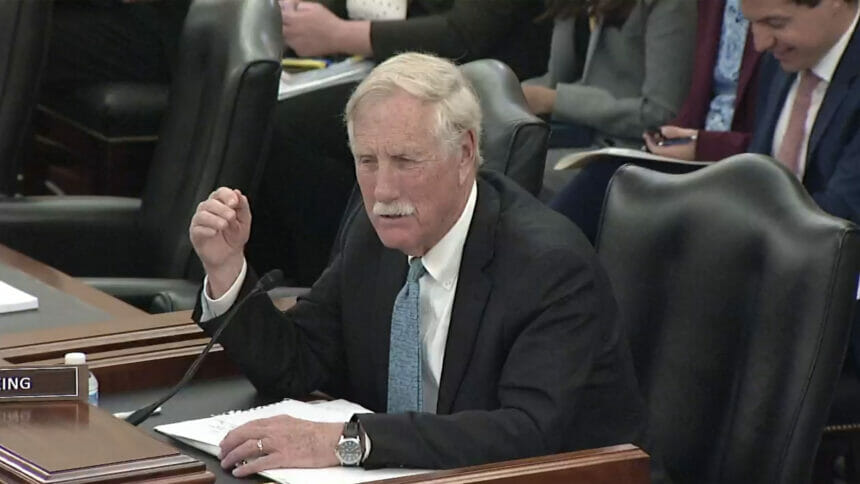
Sen. Angus King (I-ME) (pictured) pointedly questioned an official from the Centers for Medicare & Medicaid Services about the looming mandate during a hearing last week in the US Senate Committee on Veterans’ Affairs,
“You’re not serving veterans if a home closes because they can’t meet the staffing standards because they can’t find the people,” King said to Jonathan Blum, CMS’ principal deputy administrator. “Let’s get real here. Don’t tell me you’re improving service to veterans when you just said we’re going to see nursing homes close.”
Blum acknowledged that he misspoke, clarifying that, “What we want to see is a nursing home force that is more stable.”
For months now, though, providers throughout the country along with state and national associations that represent the industry have warned that a staffing mandate would further exacerbate staffing shortages, which would result in the loss of more beds and entire facilities shuttering.
CMS is expected to release within the next 10 days a mandate that sector observers say would likely call for a minimum of about 4.1 hours of care per resident per day. A number of states have staffing requirements with requirements that range from directives on the number of hours required by specific nursing specialties to more, general daily minimum.
A study commissioned by the American Health Care Association found that the mandate would require an additional 190,000 workers on top of the approximately 200,000 lost during the pandemic and cost $11 billion annually.
The sector picked up a key ally last week when Rep. Cathy McMorris Rodgers (R-WA), chair of the House Energy and Commerce Committee, announced during the association’s annual Congressional Briefing that she opposes the mandate. She characterized the forthcoming rule as “threatening to undermine care and safety” since many facilities would not be able to comply, McKnight’s Long-Term Care News reported.
Carla Wilton, chief operations officer of Immanuel Lutheran Communities in Montana, noted in her testimony at Wednesday’s senate hearing that the long-term care facility is paying CNAs nearly $20 an hour. She noted that the state has lost nearly 20% of its nursing home workforce.
“Sometimes we were unable to admit new residents due to our inability to care for them because of our low staffing numbers,” she told the committee. “We raised staff wages almost 25% across the board, and for the first time in our organization’s 65-year history, we brought in agency staff.”
Veterans’ Affairs Committee Chair Jon Tester (D-MT) and a dozen other senators representing rural states sent a letter in January to Centers for Medicare & Medicaid Services Administrator Chiquita Brooks-LaSure asking her to hit the brakes on a staffing mandate that would “undermine access to care for patients.” Tester also tweeted. “Most folks in DC don’t get rural America, so it’s my job to stand up to bureaucrats that try to impose one-size-fits-all solutions on Montana.”




