Since before the first shots of vaccine went into arms, health experts and federal officials have been pitching the idea of boosters as a way to stymie COVID-19 as it mutates.
Much of the initial chatter focused on a six-month window before decreased protection, a timeline that is beginning to worry some long-term care advocates. Seniors in congregate settings were among the first in the country to receive their shots — some as early as December — meaning, the clock could be running out on critical antibodies.
Any boosters would need to be approved by the Food and Drug Administration and recommended by the Centers for Disease Control and Prevention before they could be distributed to seniors, who are especially vulnerable to COVID’s asymptomatic spread.
“The shame of this is that when COVID-19 runs rampant in a nursing home, the mortality rate is significant,” Mike Wasserman, M.D., past president of the California Association for Long Term Care Medicine and part of the federal body that developed COVID vaccine-recipient protocols, told ABC News this week. “Hence, if and when the residents’ immunity wanes, we must be on high alert, lest we relive the horrors of the past year.”
The true challenge is that no one yet knows how long immunity might last, and if that could vary by sub-population. Studies publicized in April showed both the Pfizer and Moderna two-dose vaccines are offering significant protection past the six-month mark in trial participants.
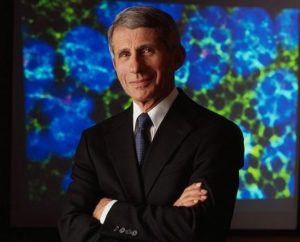
Testifying before a Senate subcommittee this week, U.S. infectious disease expert Anthony Fauci said boosters would most likely be needed between six months and a year.
“I don’t anticipate that the durability of the vaccine protection is going to be infinite,” Fauci said. “It’s just not. So I would imagine we will need, at some time, a booster.”
Pfizer CEO Albert Bourla has said a booster shot could be needed as soon as September for the earliest vaccine recipients.
The big questions are: How will nursing homes get their next round of shots if they again need them en masse, and how well will the reporting mechanisms offered by the CDC (whose use is now mandated by the Centers for Medicare & Medicaid Services) be able to identify which residents need shots, and when.
“We learned that nursing homes weren’t prepared for the pandemic and there is a lot of work to do to improve the quality of care in nursing homes,” Wasserman said. “We must start planning now.”
Toby Edelman, senior policy attorney for the Center for Medicare Advocacy, told ABC the responsibility to prepare for booster shots lies with facilities, although many are not equipped to or allowed by their states to store or distribute vaccines.
“Nursing homes should absolutely be planning for booster shots, if those become medically necessary and appropriate,” Edelman said. “The COVID-19 pandemic made clear the critical importance of facility leadership anticipating and planning for contingencies.”
Amid all the questions, there is some good news. Researchers reported in Nature Wednesday that individuals who had a mild case of COVID-19 will probably make antibodies against the virus for most of their lives. Immunologists said the immune response created by the combination of a previous infection and a vaccine is typically strong enough that it can fight virus variants.
And that could mean seniors who had COVID and a first-round vaccination may never need a booster.




