
A national analysis finds that nearly half of US nursing homes would not meet a daily, 3.5-hour nurse staffing requirement and just 29% would meet a standard of 4.0 hours.
The work from KFF exposes the challenge that nursing homes will have if the long-anticipated federal staffing mandate from the Centers for Medicare & Medicaid Services requires 4.1 hours of direct care per resident per day, as some sector observers have predicted.
National nursing home advocates and providers in nearly every state have been warning that severe workforce challenges will hinder compliance, if not make it impossible.
“While [nursing homes] provide care to an older, frail and disproportionately female population, there have been long-standing concerns about insufficient staffing in nursing facilities and its impact on quality,” the analysis said. “The high mortality rate in nursing facilities during the COVID-19 pandemic highlighted and intensified the consequences when staffing levels are low and quality suffers.”
The analysis pointed to a March 2023 report from the Government Accountability Office that found “inadequate staffing made it difficult for nursing homes to adhere to proper infection prevention and control practices.”
45 states have own staffing rules
Forty-five states and Washington, DC, have their own minimum staffing requirements, but only the District of Columbia requires 4.1 hours of care per day.
“They’re tired. They’re burned out. They’re physically exhausted, and even committed people in this industry will turn around and say, ‘I don’t know how much longer I can do this,’” Tina Sandri, CEO of Forest Hills of DC, told NPR, per a release from the American Heath Care Association/National Center for Assisted Living.
Sandri said finding certified nursing assistants is one of the biggest challenges, with four of five people who express interest in the job ghosting on interviews.
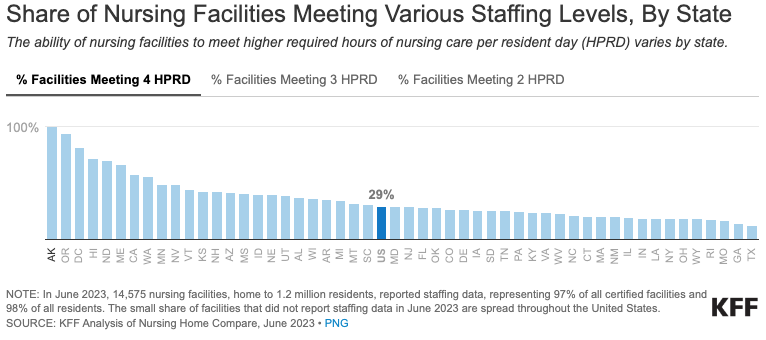
The KFF analysis found that nearly all nursing homes would be able to meet a standard of 2.5 hours or fewer and 85% would be able to staff at 3.0 hours of care per resident per day. But 45% could not meet 3.5 hours and just 29% have the staff to meet 4.0 hours.
There are variations in facilities meeting standards depending on the state, as well, with just 12% of facilities in Texas capable of meeting 4 hours per day of direct care, but all facilities in Alaska would be in compliance.
Who counts matters
A wildcard in the expected federal rule is whether it will specify types of nursing specialties that could be used to meet the minimum, which will complicate the situation. State rules vary with some requiring facilities to meet a general description of nursing hours per day, while others, such as New York, write into the rule who does what. No less than 2.2. of New York’s 3.5 hours must be performed by a certified nurse aide, for example, and no less than 1.1 hours must be performed by a registered or licensed practical nurse.
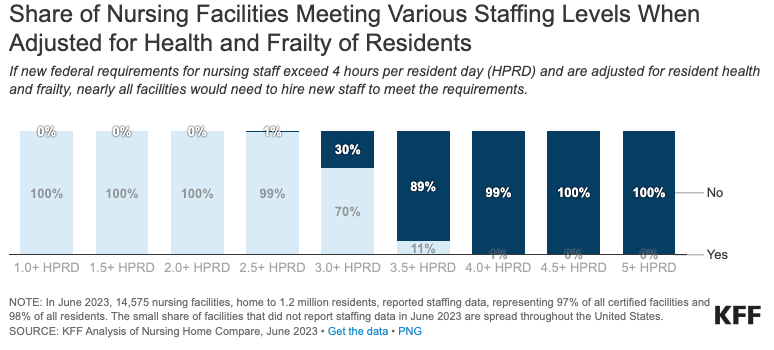
“If the proposed rule includes requirements related to the types of nurses facilities must employ (and the hours they must work) or adjusts the number of required nurses based on patient health and frailty, fewer nursing facilities would meet a given requirement than are shown here,” KFF wrote.




