

Several nursing home advocacy organizations have met with the White House Office of Management and Budget in recent days, angling to change the proposed minimum staffing rule that could be issued in final form at virtually any time.
An OMB calendar shows consumer and worker groups are just as intent on bending the ears of the policy wonks ironing out any final wrinkles in the final rule the Centers for Medicare & Medicaid Services envisions.
Providers feel the stakes couldn’t be higher.
The American Health Care Association met virtually Thursday with OMB, as well as officials from the Department of Health and Human Services and the Centers for Medicare & Medicaid Services. Three of the organization’s top government affairs leaders, its top clinical expert and two board members hammered home common themes during their meeting, keying up the proposed rule’s threat to rural providers and sharing the latest federal data on sustained losses of skilled nursing workers since the pandemic.
Nate Schema, CEO of the Good Samaritan Society, outlined how his organization had closed 14 nursing homes since the pandemic, “primarily due to challenges hiring staff in rural areas.” Sarah C. Schumann, vice president of operations for Brookside Inn, told OMB how a mandate could harm her small, family-owned skilled nursing business in Castle Rock, CO.
“The stories of passionate providers painted a clear picture of the unrealistic expectations and unintended consequences of this mandate, and we hope their stories will resonate as the administration determines its next steps,” Clif Porter, AHCA’s senior vice president of government relations told McKnight’s Long-Term Care News in a statement Monday.
“Ultimately, we are urging the administration to heed the concerns of stakeholders and members of Congress from both sides of the aisle and not move forward with this rule due to the adverse impact on access to care for our nation’s seniors,” Porter added.
LeadingAge, the provider association comprising nonprofit operators, met with OMB on March 28.
“Using staffing and labor cost data, we emphasized the staffing mandate as proposed will not be implementable and will effectively limit access to mission-driven nursing home care by older adults,” a LeadingAge spokeswoman told McKnight’s Monday. “We also brought forward solutions, including current legislation we support to expand the aging services workforce.”
Several nursing home associations also have used the meetings to remind OMB and CMS of a late February letter to the House Ways & Means Committee that included signatures from more than 1,000 organizations urging passage of the Protecting Rural Seniors’ Access to Care Act. The bill would thwart CMS’ ability to put the staffing regulations into play.
More than one side heard from
The Nursing Home Reform Coalition met with OMB on the same day as AHCA. That group included a swath of organizations and individuals who have rallied behind staffing standards — including several that said CMS did not demand enough direct-care hours in its proposed rule.
Among them were AARP; the Long Term Care Community Coalition; the National Consumer Voice for Quality Long-Term Care; the National Association of Ombudsman; and Charlene Harrington, RN, PhD, the University of California San Francisco professor emeritus who has long championed a 4.1-hour direct care daily nursing requirement.
Sam Brooks, director of public policy for Consumer Voice, told McKnight’s the group reiterated its desire for “a strong minimum staffing rule based on scientific evidence.”
“We urged that the rule reflect the reality that thousands of nursing homes, mostly nonprofit, provide more than adequate staffing every day,” Brooks said. “We also noted that a staffing standard, along with increased financial transparency and accountability, would force the industry to create better jobs to address the retention crisis in nursing homes.”
That coalition isn’t the only one weighing in on the jobs that could be created by the final version of a nursing home staffing mandate. More than half of the SEIU’s membership is in long-term care. The union has scheduled its own meeting with the OMB for this Friday, while the AFL-CIO met with officials on April 2.
The final version of the CMS staffing rule arrived at OMB for a final review March 1. Most rules are reviewed within 90 days.
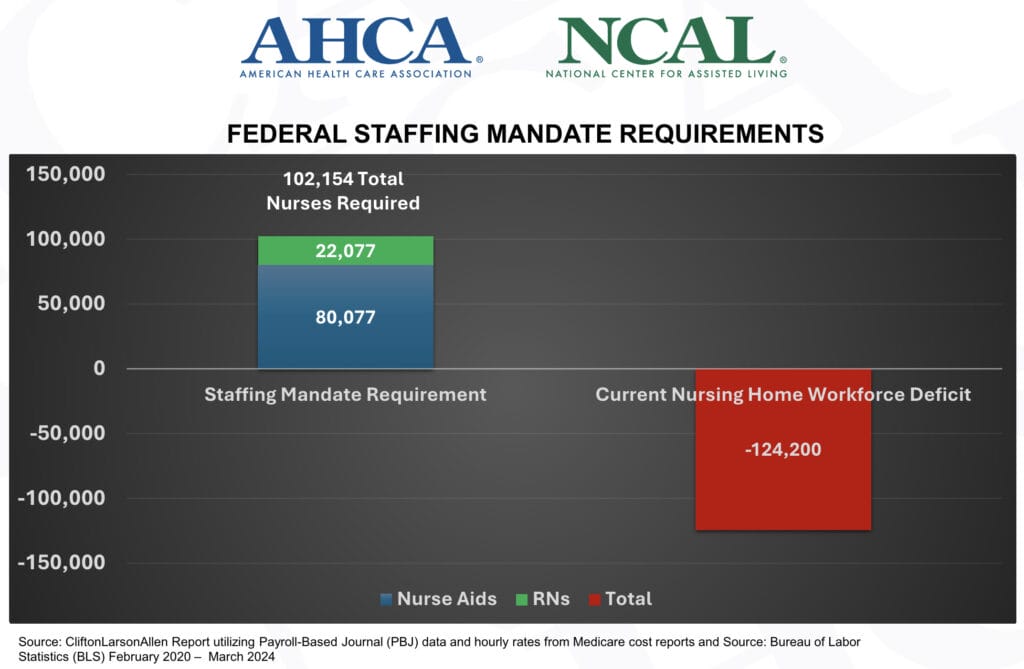
As proposed last September, the mandate would require round-the-clock registered nurse coverage as well as setting hourly minimum standards for aides and RNs. Providers have said all along those marks would be impossible to meet because nurses simply aren’t available. They’ve also objected to the possible cost, which one estimate has shown could climb to $11.7 billion annually. CMS in its initial proposal committed to spending just $75 million on nurse recruitment initiatives.




