Long-term care, including access to quality skilled nursing, is “painfully inadequate” with major gaps in every state, finds an updated scorecard issued Thursday by AARP.
In its state-by-state review, AARP specifically called out nursing homes for their ongoing workforce crisis, turnover rates, allegedly inequitable care for minorities and the ongoing prevalence of pressure injuries. In addition, AARP leaders said states are giving less-than-adequate attention to natural disasters and the importance of nursing home emergency preparedness.
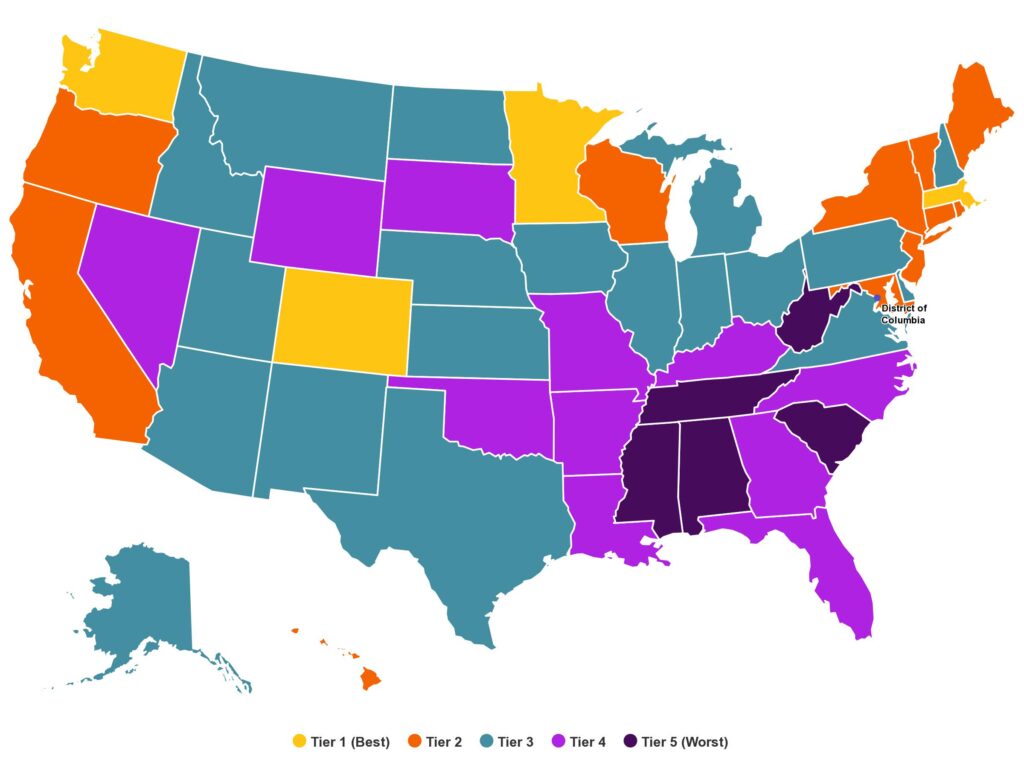
Minnesota and Washington were the top-ranked states, with relatively strong support for family caregivers and a wide range of healthcare providers and long-term care settings. All of the lowest performing states were in the Southeast, with Alabama and West Virginia at the bottom.
AARP researchers identified wage gaps that continue to make it hard for providers to attract and retain direct care workers, who make less than they would in comparable positions in other industries. Wage shortfalls ranged from $1.56 to $5.03 per hour, with New York, California, Texas, Louisiana, and Washington, DC, offering the least competitive wages. The report found the highest average turnover rates in Montana, Vermont and New Mexico.
AARP issues the scorecard every three years. With the 2020 version based on pre-COVID indicators, this is the first to capture the pandemic’s influence on long-term care supports and services, in which AARP includes informal family caregiving.
“COVID-19 tested our long-term care systems nationally and most states failed, but we do believe there’s a silver lining,” Susan Reinhard, senior vice president of the AARP Public Policy Institute said during a Thursday press conference. ”In today’s scorecard, you’ll have examples of states that are outperforming others and they can provide a roadmap for progress across the country.”
The 2023 scorecard includes 20 new indicators that show how states compare in key areas related to workforce, nursing home safety and quality, programs targeted to people with disabilities (exclusively or in addition to older adults), housing, transportation, and performance across different racial and ethnic groups. In all, there are 50 indicators using data from the Centers for Medicaid & Medicare Services, the Census Bureau’s American Community Survey and the Bureau of Labor Statistics and more.
Reinhard noted that the rankings tied closely to states’ support for family caregivers, through generous leave policies or tax credits. A state’s ranking also tended to hew closely to how supportive its Medicaid payment policies are.
“It’s the strongest correlation in the performance in general,” Reinhard said. “It’s showing that you’re paying attention to the people that are providing the care and where the care is given. Medicaid policy is extremely important in performance.”
Reinhard and Rita Choula, senior director of caregiving for the AARP Public Policy Institute, focused many of their comments on non-professional caregiving. Generous support for home- and community-based services helped move some states into high tiers in the report, which divided grouped states into five performance levels.
Regarding nursing homes specifically, the report called out staffing disparities in facilities that serve a high share of minority residents. Residents of nursing homes with high admissions of Black residents receive almost 200 fewer hours of care per year compared to residents of nursing homes with high admissions of white residents, AARP said.
Reinhard also singled out nursing homes for the lack of emergency planning. Only nine states have enhanced hazard mitigation plans for natural disasters and other emergencies to address the needs of vulnerable older adults, although she noted that states that work with the Federal Emergency Management Authority to develop such plans can net extra funding.
The report recommended that states:
- Bolster the nursing home and in-home care workforce, with improved recruitment and training, increased pay, and an expanding ability of trained nurses, aides and community health workers to take on new aspects of care. In addition, AARP encouraged states to enact and enforce nursing home staffing and other care standards.
- Expand the use of innovative, effective models for nursing homes, such as Green House Homes, that can improve quality of care and quality of life.
- Address inequities by making investments that close “staggering” gaps in access to quality care and facilities and staffing shortages.
“We know that there’s no magic bullet to reform and modernize long-term care systems overnight,” Reinhard said. “But the data in our scorecard report can guide not only governors and state legislators on smart policies and initiatives for the future but provide the federal government with the window into what works and why.”



