
A fresh report from a Congressional advisory panel Wednesday revealed wide fluctuations in state Medicaid rates, findings that come as federal regulators are weighing a staffing mandate and increasing their scrutiny of nursing home owners.
Average base Medicaid payment rates for nursing facility services varied considerably, from 62% to 182% of the national average, after adjusting for differences in area wages and resident acuity, according to an issue brief from the non-partisan Medicaid and CHIP Payment and Access Commission.
MACPAC staff looked at costs and reimbursements from 2019 (pre-COVID) as a way to better evaluate how much care that state funding is actually covering.
“Costs have historically been used to assess Medicaid nursing facility payments, but they are an imperfect measure of what facilities should be paid,” the brief noted. “On one hand, costs for some facilities may be too low to meet resident care needs, especially if the facilities are understaffed. On the other hand, some facilities may report costs that are higher than what would be needed to operate the facility efficiently and economically.
“For example, in recent years, there have been concerns that some facilities that are part of larger chains have used related-party transactions to inflate costs reported on facility-specific cost reports by including costs incurred by other entities that are part of the overall chain.”
While a MACPAC spokeswoman said the variability of SNF payments had long been of interest to the commission, the findings also bolster recent provider concerns about lagging state reimbursement. They come as the Centers for Medicare & Medicaid Services has been putting pressure on states to better support long-term care, a shift the American Health Care Association has said must happen before any proposed staffing mandate is implemented.
Less staff, less quality?
MACPAC staff found that facilities serving a high share of Medicaid-covered residents generally have lower base pay rates but also have lower facility costs, “in part because they generally have lower staffing levels than other facilities.”
Measures of base payments relative to costs varied widely, ranging from less than 70% of costs for 15% of facilities to more than 100% of costs for 19% of facilities. The median Medicaid base payment rate in 2019 was 86% of costs.
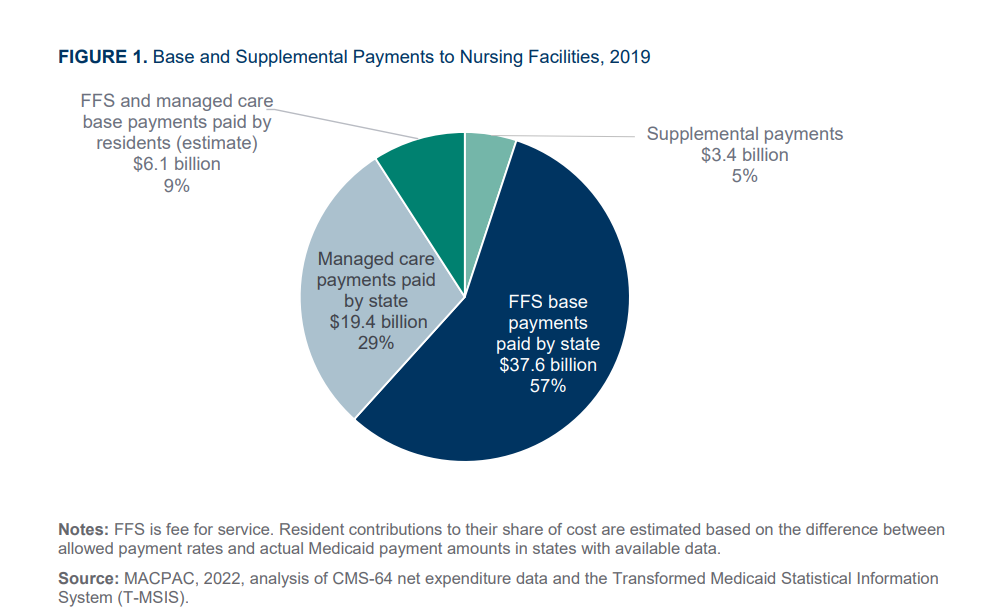
Fewer than half (23) of the states made lump-sum supplemental payments, which were generally based on the difference between Medicaid fee-for-service base payments and the amount that Medicare would have paid for the same service.
In several areas, the issue brief ties findings to concerns about staffing levels, care quality and transparency of related parties.
For instance, it noted that average costs of care for Medicaid-covered residents were lower than the average costs per day for all nursing facility residents. Even after researchers made adjustments for acuity, facilities that had a higher share of Medicaid beneficiaries still reported lower costs on average than other facilities.
“Some of these lower costs may be explained by the fact that facilities that serve a higher share of Medicaid-covered residents generally have lower staffing levels than other facilities,” the brief said, adding that 49% of facilities serving the highest share of Medicaid residents had a 1- or 2- star staffing rating in 2019.
But the analysis did not find a “clear relationship” between Medicaid payments rates and staffing.
Staff did report that facilities with higher staffing ratings also paid higher average hourly wages to direct care nursing staff.
More facility-level data sought
Overall, nursing facility services paid for by Medicaid accounted for 80% of total nursing facility costs in 2019, according to Medicare cost reports. Ancillary costs, such as therapy, not paid for by Medicaid were excluded. Additionally, MACPAC found that about 6% of reported costs were for other expenses that are typically not covered by Medicare or Medicaid.
Authors expressed frustration with varying staffing levels and other practices that obscured the true costs of caring for long-stay residents.
“We were not able to examine the effects of related-party transactions and other practices that may artificially inflate the costs reported on Medicare cost reports,” they wrote. “This analysis reinforces MACPAC’s long-standing concern about the need for additional payment and financing data at the facility level, especially for supplemental payments. Such data are needed to provide a complete understanding of all types of Medicaid payments to nursing facilities, which can help inform assessments of the link between payment and access, quality and value.”




