

Earlier this month, new research comparing RUGs IV therapy minutes versus PDPM minutes was released by the JAMA Health Journal. I was shocked – but not by the data. That mirrored some of the information we received in the SNF Proposed Rule for FY 2022 showing outcomes were not harmed by an overall reduction in therapy minutes.
What was shocking was the conclusion that these results somehow prove that RUGs IV therapy minutes were artificially inflated.
I would argue instead that therapists were nimble and worked very hard to fine tune their skills to be able to achieve the same goals with reduced therapy minutes and resources during the transition to PDPM. In a value-based world, therapists should be lauded for their achievements under PDPM, rather than scolded for typical practice under RUGs IV, which was by the way, equally successful in achieving outcomes.
Let me tell you a story from five years ago about the evolution of therapy practice IRL – In Real Life. In a large urban SNF, we worked with an ACO who told the SNF therapy department that they couldn’t see any patients longer than two weeks, unless the ACO’s medical director approved it.
In two years and after hundreds of patients, the director only approved one patient to stay longer than 14 days. This was during the era, as I’m sure you will remember, when a 30-day SNF stay was trending.
But we buckled down and collaborated to figure out how we could change our delivery of service to achieve successful outcomes and safe patient transitions.
We were able to do it, and in a few years, we demonstrated the ability to achieve virtually the same outcomes with less than half the length of stay. And do you know what I learned from this? Therapy could do better, and we did.
But it didn’t just happen.
We didn’t just cut the SNF stay in half and magically achieve those outcomes. We rethought our entire delivery of services. We re-examined which CPT codes we were using, how much focus we had on functional tasks, what could be adjusted or eliminated in our efforts to provide the highest quality of therapy we could, and more.
The same thing happened with therapy minutes under PDPM. We once again determined how we were going to serve the patients well under this new payment structure, while reimagining the role of the SNF therapist under PDPM as a care provider and navigator and integrating therapists into the care team while tearing down silos.
It wasn’t easy and it wasn’t overnight. So, the conclusions the researchers had that under RUGs IV, “There were targets therapists were steering to hit, to maximize reimbursements, and they were very successful in doing that,” is inaccurate. Therapists were following industry standards, best practice at the time, and quite frankly, what they had been taught to do by their clinical mentors.
Therapists have yet again learned to do our job better, with even further reduced resources through the transition to PDPM. We should not be punished for fewer therapy minutes through PDPM parity adjustments.
The SNF Proposed Rule for FY 2022 admits that therapy outcomes didn’t decline with an adjustment in minutes, and that PT and OT didn’t cost CMS any more than predicted.
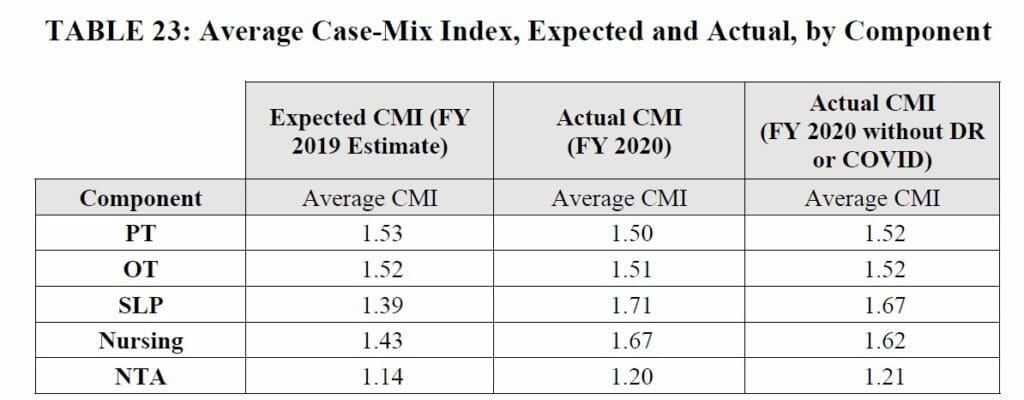
We can and must advocate now so that these PDPM parity adjustments do not result in reduced therapy reimbursement, especially for PT and OT. Therapy has made amazing progress and achieved results with a tighter reimbursement (and fewer therapy minutes) than before.
But you can only squeeze so much juice out of a lemon before there is no more to squeeze.
Melissa (Sabo) Brown, OTR/L, CSRS, CDP, is the Chief Operating Officer of Gravity Healthcare Consulting. She is an Occupational Therapist with almost 20 years of experience in skilled nursing, CCRCs and home health.
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.





