
Much has changed since the 1918 flu pandemic, when fewer than 35% of US households were connected by telephones. We have since evolved to be continuously connected, and our medical knowledge and abilities have grown to cure more often than palliate. Yet the mechanism of healthcare delivery — a physician examining a patient in an office or bedside — had remained relatively static 100 years later.
Such inertia was disrupted by the arrival of COVID-19, with telemedicine becoming a household concept seemingly overnight to provide safer, socially-distanced care. Virtual visits have ballooned from 9% of patient interaction pre-pandemic to 51% at their peak.
Skilled nursing facilities, hit particularly hard by the pandemic, present an opportunity to create novel virtual care platforms that can not only alter workflows, but actually improve outcomes. Under normal circumstances, SNF patients face challenges accessing specialty care, with infrequent appointments and a significant transportation burden. Further, this population is typically high-risk with multiple comorbidities and post-hospitalization, representing a need for high-touch, yet scalable, care.
Heartbeat Health, a digital clinical care company specializing in cardiovascular care, has been providing overnight virtual care for Cassena Care, a group of 11 skilled nursing with more than 3,500 beds in the greater New York City area. The partnership resulted in a 39% reduction in emergency room visits over several months. The downstream avoidance of unnecessary medical interventions and hospitalizations, along with the corresponding reduction in costs, represents a major victory for patients and payers alike. They are exploring how a similar model results in readmission reduction for the highest risk cohort, those living with heart failure.
Bringing specialty care to the SNF setting through telemedicine will further bend the cost curve and transform outcomes. The pandemic has already catalyzed the 2021 Physician Fee Schedule, with the Centers for Medicare & Medicaid Services reducing frequency limitations on telehealth services in nursing facilities.
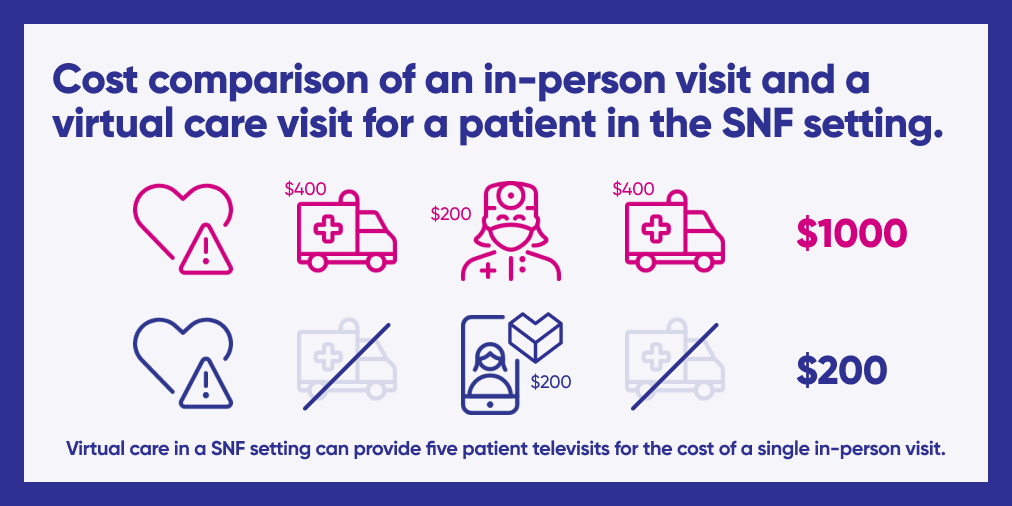
This shift represents an opportunity to further prove out value in virtual care beyond merely increasing utilization. Healthcare spending can also be reallocated to cover actual care delivery rather than the logistics of this care: money spent on transportation to a single in-person visit can be redirected to more frequent virtual touchpoints.
Despite the havoc wreaked by COVID-19, it likely exposed a major opportunity to improve outcomes and reduce costs for patients in the SNF setting. The promising early results of a virtual cardiology program in a SNF setting pave the way for future study as we continue to craft specialty telehealth for populations in need.
Nodar Janas, M.D., is medical director at Margaret Tietz Nursing & Rehabilitation in Queens, NY. Jana Goldberg, M.D., is a cardiologist and medical director of Heartbeat Health. Jeff Wessler, M.D., is a cardiologist and CEO of Heartbeat Health. Daniel Friedman, M.D. is Heartbeat Health’s product manager.




