
Tuesday evening, I began the painful eye roll-inducing process of organizing and sorting school supplies for our official start today.
Two high schoolers, two middle schoolers, and one lower schooler = five accompanying lists of essential items required to ensure a successful year ahead.
Clorox wipes – 1 container; colored pencils – 1 box Crayola (12 count); crayons – 1 box (48 count); dry eraser markers – 1 box (Expo low odor preferred); glue – 1 bottle of Elmer’s no-run washable white school glue; markers – 2 boxes of broad line Crayola Classic (10 count); pencils with erasers – 2 large packs of Ticonderoga 24 plain yellow #2 pencils; Post-it Notes – 6 each (or 1 pkg. of 6) of 1.5″ x 2″ and 1 pkg. of 6 of 3″ x 3″ – any color; Maped/Helix Ruler Plastic Standard/Metric Ringbinder Shatter-Resistant w/Holes Transparent Assorted; Fiskars Scissors Student Pointed 7″; Writing utensils; TI-83 calculator or above; Highlighter Chisel Tip Yellow (EACH) Made in USA; Three-ring binder (1.5”) or a section of a larger binder to hold Powerpoint presentations and quizzes.
The specificity and care taken to create these lists must mean that without them, the kids are all sure to fail!
Right…
As I begin unpacking the little boys’ (aka Isaac and Joseph) backpacks from last year, I soon realize those two knuckleheads never opened or unpacked ANY of their school supplies from last year. They literally packed around unopened binders, pens, pencils, dividers, colors, etc… and somehow managed to survive.
By sharing, I also realize I’m giving away the fact that I am not a backpack or homework-checking mom but assume you all know that about me at this point.
Standardization here would be fantastic, however unreasonable with three different school settings and various needs at each level based on age, cognitive status, ability to sit still for longer than 15 minutes, and so forth.
While challenging my struggles are nothing in comparison to the daunting task given to the CMS Technical Expert Panel TEP for the Refinement of Long-Term Care Hospital (LTCH), Inpatient Rehabilitation Facility (IRF), Skilled Nursing Facility (SNF)/Nursing Facility (NF), and Home Health (HH) Function Measures whose work with Abt Associates and Acumen was recently posted for public view.
What was this group’s aim you ask?
Project Overview
- The Centers for Medicare & Medicaid Services has contracted with Acumen LLC and Abt Associates to develop quality and cost measures for use in the IRF, LTCH, SNF, and HH QRPs and the Nursing Home Quality Initiative (NHQI).
- The contract Acumen LLC operates under is the Quality Measure & Assessment Instrument Development & Maintenance & QRP Support for the Long Term Care Hospital, Inpatient Rehabilitation Facility, Skilled Nursing Facility, Quality Reporting Programs, & Nursing Home Compare (75FCMC18D0015/Task Order 75FCMC19F0003).
- Abt Associates operates under the Home Health and Hospice Quality Reporting Program Quality Measures and Assessment Instruments Development, Modification and Maintenance, & Quality Reporting Program Oversight Support contract (75FCMC18D0015/Task Order 75FCMC19F0001).
- As part of its measure development process, Acumen LLC and Abt Associates convenes groups of stakeholders and experts who contribute direction and thoughtful input to the measure developer during measure development and maintenance.
Project Support
- Under this project, the PAC QRP Support team supports CMS in the development and maintenance of quality measures for use in the IRF, LTCH, SNF, and HH QRPs and the Nursing Home Quality Initiative (NHQI).
- These measures are designed to improve care quality and to enable Medicare beneficiaries to make informed choices when selecting a healthcare provider. The suite of PAC QRP measures covers several domains relevant to care quality, including function – a dimension of care that is especially salient to each of the PAC settings. Over the last decade, CMS has introduced several measures addressing function.
Project TEP Role
- To ensure these and any newly developed function measures meet CMS program requirements and goals while maintaining high levels of scientific acceptability, the PAC QRP Support team convened a Technical Expert Panel (TEP).
- The PAC QRP Support team sought guidance on specifications for a cross-setting functional outcome measure to implement across PAC QRPs. The TEP meetings focused on finalizing the GG items to use for measure construction, discussing the method to use to address Activities Not Attempted (ANAs), considering how social risk factors impact patient outcomes, and reviewing risk adjustment strategies.
Section GG
To begin, the report highlights the fact that Section GG of each PAC assessment instrument includes standardized patient assessment data elements that measure functional status.
For those of you who have been asking, “Is Section GG our PAC outcome measure?” please pay attention to what follows.
The functional status data elements used to calculate the PAC QRP function measures capture a patient’s capacity to perform daily activities related to self-care (GG0130) and mobility (GG0170) at admission/start of care (SOC)/resumption of care (ROC)2 and discharge.
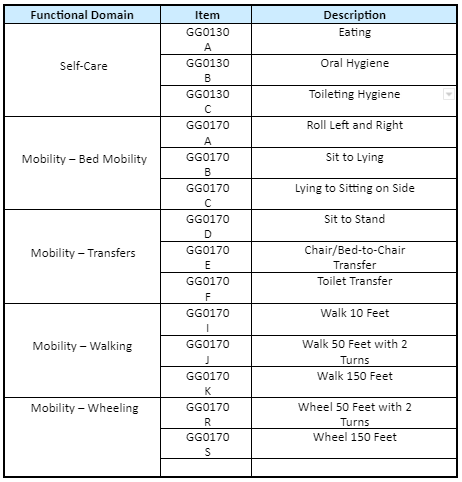
Table 3 reports the GG items currently available across all PAC settings (see Appendix B for full list of GG items).
Table 3. GG Items Available Across PAC Settings
Furthermore, there are currently six function measures across the PAC QRPs based on section GG items, including one process measure and five functional outcome measures (Table 5).
Table 5. PAC QRP Function Measures
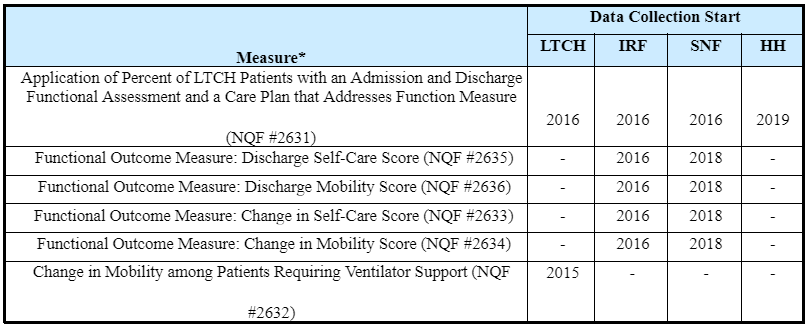
Table B1. Self-Care Assessment Item Data Collection Start Dates
| Item | Description | IRF | LTCH | SNF | HH |
| GG0130A | Eating | 2016 | 2016 | 2016 | 2019 |
| GG0130B | Oral Hygiene | 2016 | 2016 | 2016 | 2019 |
| GG0130C | Toileting Hygiene | 2016 | 2016 | 2016 | 2019 |
| GG0130D | Wash Upper Body | – | 2016 | – | – |
| GG0130E | Shower/Bathe Self | 2016 | – | 2018 | 2019 |
| GG0130F | Upper Body Dressing | 2016 | – | 2018 | 2019 |
| GG0130G | Lower Body Dressing | 2016 | – | 2018 | 2019 |
| GG0130H | On/Off Footwear | 2016 | – | 2018 | 2019 |
Table B2. Mobility Assessment Item Data Collection Start Dates
| Item | Description | IRF | LTCH | SNF | HH |
| GG0170A | Roll Left and Right | 2016 | 2016 | 2018 | 2019 |
| GG0170B | Sit to Lying | 2016 | 2016 | 2016 | 2019 |
| GG0170C | Lying to Sitting on Side | 2016 | 2016 | 2016 | 2017 |
| GG0170D | Sit to Stand | 2016 | 2016 | 2016 | 2019 |
| GG0170E | Chair/Bed-to-Chair Transfer | 2016 | 2016 | 2016 | 2019 |
| GG0170F | Toilet Transfer | 2016 | 2016 | 2016 | 2019 |
| GG0170G | Car Transfer | 2016 | TBD | 2016 | 2019 |
| GG0170I | Walk 10 Feet | 2016 | 2016 | 2018 | 2019 |
| GG0170J | Walk 50 Feet with 2 Turns | 2016 | 2016 | 2016 | 2019 |
| GG0170K | Walk 150 Feet | 2016 | 2016 | 2016 | 2019 |
| GG0170L | Walk 10 Feet – Uneven Surface | 2016 | TBD | 2018 | 2019 |
| GG0170M | 1 Step (Curb) | 2016 | TBD | 2018 | 2019 |
| GG0170N | 4 Steps | 2016 | TBD | 2018 | 2019 |
| GG0170O | 12 Steps | 2016 | TBD | 2018 | 2019 |
| GG0170P | Picking Up an Object | 2016 | TBD | 2018 | 2019 |
| GG0170R | Wheel 50 Feet with 2 Turns | 2016 | 2016 | 2016 | 2019 |
| GG0170S | Wheel 150 Feet | 2016 | 2016 | 2016 | 2019 |
Activities Not Assessed (ANA)
For all my “If you didn’t code it, it didn’t happen” crew out there, you will appreciate this discussion.
For the functional outcome measures currently implemented in the LTCH, IRF, and SNF QRPs, all ANA codes are recoded to 1 (dependent) when calculating measure scores.
This approach assumes that all ANAs equate to scenarios where patients are fully dependent for a particular activity, however ANAs do not always reflect dependence on a function activity.
To resolve this issue, the TEP was presented with multiple options including
- Current Recode: all dependent
- Rescale: An alternative solution to the current recode method is to rescale the assessed items (i.e., non-ANAs) in a way that counterfactually creates a score as if it were based on the full set of items.
- Statistical Imputation: Another approach to handle ANAs is to use the information collected through the assessments (e.g., patient demographics, such as age, and comorbid conditions) to impute the missing scores
- Alternative Suggestions: (1) a bootstrapping analysis to obtain bias/error estimates and (2) an incentive simulation analysis
Social Risk Factors
The PAC QRP Support team also reviewed a common list of SRFs in the conceptual model for PAC that have the potential to, directly or indirectly, impact patient outcomes.
Bolded items indicate currently available data and italicized items indicate data elements that will be available in the future.
- Socioeconomic Position
- Income, Education, Dual Eligibility, Wealth
- Race, Ethnicity, and Cultural Context
- Race and Ethnicity, Language, Nativity and Acculturation
- Sexual Orientation and Gender Identity
- Sexual Orientation and Gender Identity
- Social Relationships
- Marital/Partnership Status, Living Alone, Social Support
- Residential and Community Context
- Neighborhood Deprivation, Urbanicity and Rurality, Housing, Transportation, Social Cohesion, Proximity to Services, Public Safety
Figure 1. Conceptual Model for Functional Outcomes in PAC
Next steps and summary
The input provided by this TEP will provide guidance to the PAC QRP Support team throughout the cross-setting functional outcome measure development effort.
Item Set for a Cross-Setting Function Measure
- The panelists agreed with removing the Sit-to-Lying item (GG0170B) from the cross- setting measure specification and adding Self-Care items (GG0130A-C). The TEP members were conflicted about removing the Walk and Wheel 150’ items. The PAC QRP Support team will conduct further analysis to inform this decision.
Imputation Methodology for Addressing ANAs
- The panelists arrived at a consensus that the current recode can be improved upon and that statistical imputation should be the method to use instead. The PAC QRP Support team will continue to refine the imputation methodology to improve performance across settings.
Impact of SRFs on Measure Scores
- The panelists expressed support of both the conceptual model presented and for further analysis. The PAC QRP Support team will conduct further analysis to understand the effects of measurable SRFs.
Testing Additional Risk Adjustment Variables
- The panelists expressed support for setting-specific risk adjustment models. The PAC QRP Support team will test incorporating additional clinically advisable and feasible risk adjustment covariates.
Renee Kinder, MS, CCC-SLP, RAC-CT, is Executive Vice President of Clinical Services for Broad River Rehab and a 2019 APEX Award of Excellence winner in the Writing–Regular Departments & Columns category. Additionally, she serves as Gerontology Professional Development Manager for the American Speech Language Hearing Association’s (ASHA) gerontology special interest group, is a member of the University of Kentucky College of Medicine community faculty and is an advisor to the American Medical Association’s Current Procedural Terminology CPT® Editorial Panel. She can be reached at [email protected].
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.





