
Ever receive the exact right message at the right time?
It happened to me last night at 9:21 p.m. EST. A simple email of thanks and kindness landed in my inbox.
A thanks, really at that time undeserved, and while I was in a panic over an errored ICD-10 coding report I had created for a training.
9:21 p.m. simple message, thank you. God bless you. Have a blessed night.
That simple message was exactly what I needed to focus on in that moment.
So, I am here to ask you today. What message does your coding say about your community?
Specifically, what does your claims data show related to use of MDS Section I0020B?
As a reminder, the RAI Manual defined Section I: Active Diagnoses intent as follows:
Intent: The items in this section are intended to code diseases that have a direct relationship to the resident’s current functional status, cognitive status, mood or behavior status, medical treatments, nursing monitoring, or risk of death. One of the important functions of the MDS assessment is to generate an updated, accurate picture of the resident’s current health status.
Steps for Assessment:
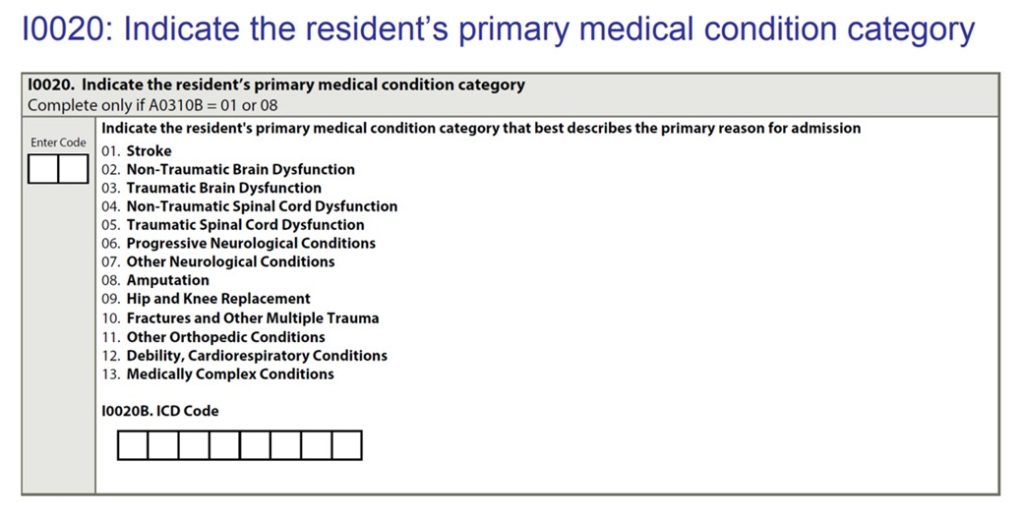
I0020 – Indicate the resident’s primary medical condition category that best describes the primary reason for the Medicare Part A stay.
I0020B – Enter the International Classification of Diseases (ICD) code for that condition, including the decimal.
Seems simplistic, right?
The right message … Mr. Smith was in the hospital for (blank) dx.
At the right time, per submissions guidelines, we code and submit I0020B with (blank) dx.
Not always.
Remember, the Centers for Medicare & Medicaid Services (CMS) clarified in its PDPM FAQs.
1.8 Is it required that the principal diagnosis on the SNF claim match the primary diagnosis coded in item I0020B?
- While we expect that these diagnoses should match, there is no claims edit that will enforce such a requirement.
1.9 Is it required that the SNF primary diagnosis match the primary diagnosis reported for the qualifying hospital stay?
- No, the primary diagnosis for the SNF stay may differ from the primary diagnosis reported for the hospital stay that serves as the qualifying hospital stay necessary for SNF coverage.
How can this be true? Why would CMS create such a mixed coding message?
Perhaps, this was done to force greater interdisciplinary team collaboration.
To express the right message, at the right time, to best serve our patients daily.
Curious as to where the nation was trending?
Below is a representation of the data on principal diagnosis for Medicare Part A SNF claims for Q2 2020 as reported by CMS Research Data Assistance Center (ResDAC).
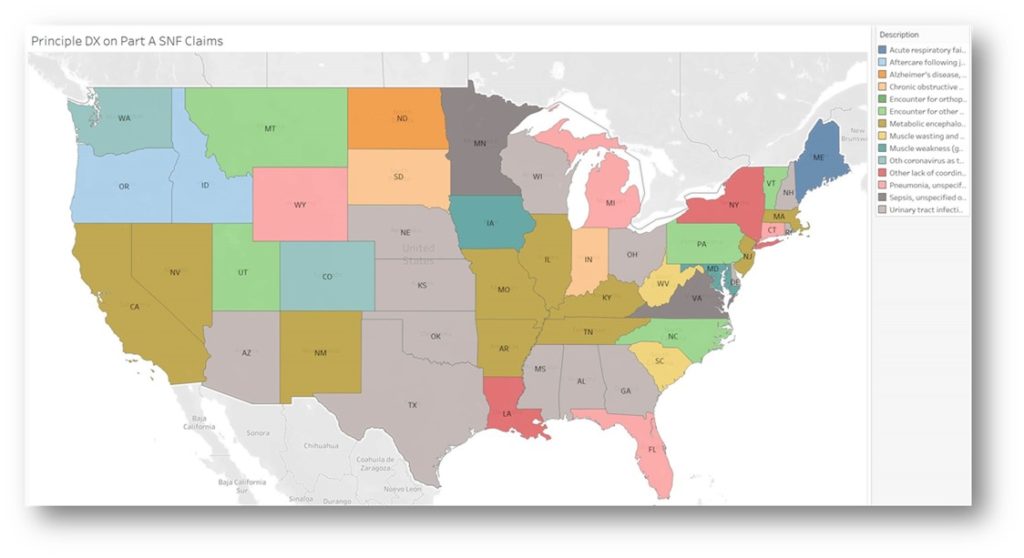
Principal Diagnosis on Part A SNF Claims Q22020, Source: CMS ResDAC
Furthermore, as we consider the impact of medical complexity on patients recovering from COVID-19 we should recognize the message our coding reflects associated with CMS 100-2 Chapter 8.
This document clarifies that, “To be covered the extended care services must have been for the treatment of a condition for which the beneficiary was receiving inpatient hospital services (including services of an emergency hospital) or a condition which arose while in the SNF for treatment of a condition for which the beneficiary was previously hospitalized.
In this context, the applicable hospital condition need not have been the principal diagnosis that actually precipitated the beneficiary’s admission to the hospital, but could be any one of the conditions present during the qualifying hospital stay.
Coding, the right message at the right time.
What message is your community’s coding communicating about you?
Renee Kinder, MS, CCC-SLP, RAC-CT, is Executive Vice President of Clinical Services for Broad River Rehab and a 2019 APEX Award of Excellence winner in the Writing–Regular Departments & Columns category. Additionally, she serves as Gerontology Professional Development Manager for the American Speech Language Hearing Association’s (ASHA) gerontology special interest group, is a member of the University of Kentucky College of Medicine community faculty, and is an advisor to the American Medical Association’s Relative Value Update Committee (RUC) Health Care Professionals Advisory Committee (HCPAC).





