

The immediate relief I felt when the Centers for Medicare & Medicaid Services issued a blanket waiver 1135 on March 13 was soon replaced with confusion and anxiety.
An 1135 waiver authorizes the Secretary of Health and Human Services to take actions normally beyond regular authority. For example, temporarily modify Medicare, Medicaid, & CHIP requirements to ensure sufficient healthcare items and services are available to meet the needs of individuals in an emergency area during a specific time period.
The “blanket” designation means that individual states and providers do not need to apply, although they may request additional flexibility.
The confusion I felt was in part due to not all 1135 waivers being the same; the COVID waiver was particularly confusing as it addressed long-standing Medicare eligibility requirements that were poorly understood to begin with.
Most waivers deal with specific locales surrounding emergencies or disasters and are unique to the situation that necessitated them. Assuming that all blanket waivers are the same, is an error — yet comparing the differences in language can be instructive. Let’s focus on the current national blanket 1135 waiver that was signed by CMS Administrator Seema Verma two weeks ago, and is retroactive to March 1, 2020.
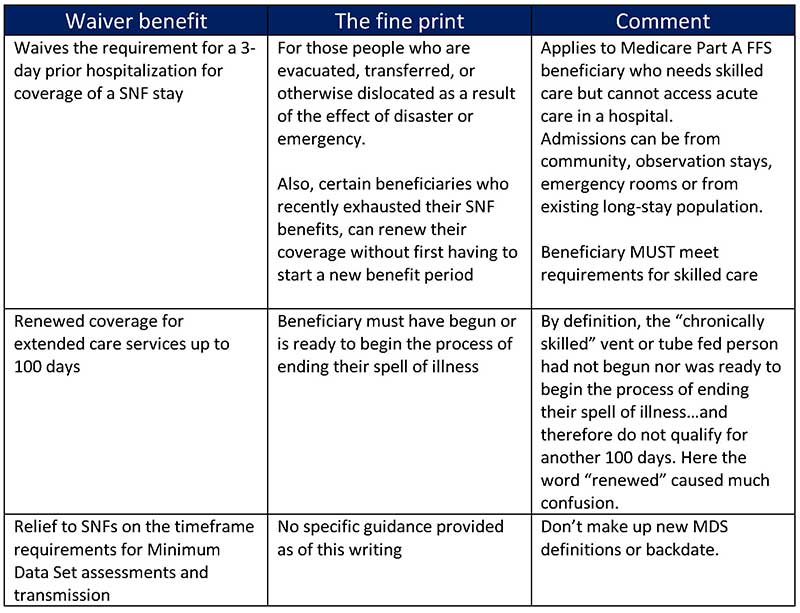
A quick summary, CMS’ COVID-19 blanket waiver:
The antidote to confusion is knowledge, but why was I feeling anxious? Then the “one-off calls, emails and questions” became a pattern that revealed a very fundamental lack of understanding about the definition of skilled care as outlined in Chapter 8 Medicare benefit policy manual. (And I can feel your eyes rolling in your head as you read this). The bottom line is this: The waiver doesn’t change the clinical criteria that defines a beneficiary for Medicare Part A services. Mic drop.
Let me share a few quotes from well-regarded colleagues to illustrate many of these points.
Marc Zimmet, president and CEO of Zimmet Healthcare (ZHSG) made this point on a recent “Waiver Call” March 23, 2020:
“The blanket waiver allows skilled care to be provided and reimbursed without a 3-day inpatient hospital stay, if the beneficiary was dislocated or are otherwise affected by the emergency. This includes those that need SNF care as a result of the emergency, regardless of whether that individual was in a hospital or nursing home prior to the emergency.” He went on to say that “The beneficiary doesn’t need to have COVID-19 but caring for them in the SNF avoids utilizing needed hospital resources.”
I had a “virtual office visit” with Michael Sciacca, chief operating officer of ZHSG. I asked him what common questions were being asked about the blanket waiver, and he shared this:
“If a patient had exhausted their current 100-day Medicare benefit and is no longer skilled, but is still within their spell of illness*, and then developed a new skilled need such as respiratory treatments or IV medications related to an acute or exacerbated chronic condition, they are entitled to a new benefit period without a 3-night hospital stay.” “With the waiver, they are entitled to a new benefit period without the 60-day break or a 3-day hospital stay.”
*A spell of illness begins with the first day of Medicare-covered (SNF) care in the facility and ends (is broken) when the resident is either: Discharged or does not require skilled care for 60 consecutive days.
Michael continued: “Another common question asked is, ‘Does the waiver allow me to convert my long-term residents who are receiving Part B therapy to Medicare Part A?’ The answer is a resounding ‘NO!’ The vast majority of these cases would not be considered acute in nature or meet the definition of skilled care. Said differently, they would not have resulted in a hospitalization under normal circumstances.”
Finally, while this writing focused exclusively on the current blanket 1135 waiver from CMS, it is not the only active waiver that exists to offer relief during this COVID-19 crisis.
“There are two other types of 1135 waivers: waivers requested by providers or groups of providers, and waivers requested by states,” explained Jay Gormley Chief Strategy & Planning Officer at MJHS, before the weekend. “As of today there are 29 approved state waivers related to the COVID-19 crisis. The vast majority of state waivers are based on ‘Checklists and Tools’ released by the Trump Administration that focus mainly on Medicaid and CHIP.
“However, some states that have submitted 1135 waivers have also included additional extensive modifications to Medicare rules,” he added. “Each provider should check with the CMS website or their local State DOH resources to see what other Medicare and Medicaid modifications may apply to them.”
Dear friends, during these unprecedented difficult and challenging days, when our commitment to quality care is most challenged, I pray for your safety and continued strength.
Steven Littlehale is a gerontological clinical nurse specialist, chief innovation officer at Zimmet Healthcare Services Group, and chief clinical officer emeritus at PointRight Inc.





