
Series Introduction
The Advancing Excellence in Long-Term Care Collaborative is a community of diverse collaborators who experienced the pandemic differently and from different perspectives. We have shared information, offered insights, supported each other and advanced initiatives and events to address the multitude of challenges experienced by residents, staff, and long-term care leaders across the United States.
Despite these challenges, the pandemic also taught us many lessons and created opportunities. The focus on the long-term care community increased public awareness of the long-standing hurdles faced by the industry. Advancing Excellence has used this opportunity to leverage our diverse perspectives to inform policymakers about effective strategies to address problems related to the pandemic and beyond. Our goal for the Biden‐Harris administration is to ensure that emerging policies and regulations incorporate clinical, ethical and operational considerations to help improve the lives of vulnerable residents and staff in post-acute and long-term care (PALTC) during these uncertain times.
Based on our commitment, we developed this series of articles, each reflecting one of our core recommendations and the rationale behind it. We have engaged expert leaders within the broad Advancing Excellence membership to author these pieces.
In this first of six installments, Chris Laxton and Patrick Luib focus on infection control. Other pieces will address person-centered care, staff stability, quality assurance and performance improvement, value-based payment, and cross-agency collaboration. We welcome you to use this content and reference our complete set of recommendations to help promote change in long-term care.
– Theresa Schmidt, for Advancing Excellence
Just as the Delta surge began to fade, flu season arrived along with colder weather. The case numbers for COVID-19 once again ticked up and, just in time for Thanksgiving, we learned of the emergence of Omicron. Most mutations of SARS-CoV-2 have no impact on viral function; however, Omicron has joined Delta, Alpha, Beta, and Gamma on the World Health Organization’s latest variant of concern.
The scientific community is still learning about this variant and what it means for the response to the pandemic, especially the severity of the disease it can cause and the degree to which it can break through vaccine protection. While this is ongoing, the Centers for Medicare & Medicaid Services (CMS) and other government agencies must continue to support nursing home residents and their families, along with nursing home staff, to implement effective infection prevention and control (IPC) practices during the pandemic and beyond.
In September, the Biden administration and Centers for Disease Control and Prevention (CDC) announced a $2.1 billion investment of American Rescue Plan funds to improve IPC activities across the U.S. public health and healthcare sectors. A week before this announcement, the Advancing Excellence in Long-Term Care Collaborative shared our policy recommendations in an open letter to the Biden-Harris administration.
One of the most immediate and urgent Advancing Excellence recommendations is to develop and implement a federal regulatory framework that addresses the root causes of IPC performance gaps in PALTC settings of care (Figure 1) and develops solutions for improvement.
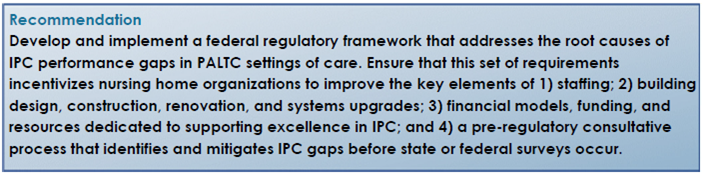
One simple staffing-related approach is to raise visibility for the important role of the nursing home medical director. The federal government should start by establishing a public-facing, national registry of nursing home medical directors, showing the board certification(s) these physicians have and which nursing homes they support.
Another would be to require a minimum level of specialized training for medical directors to effectively carry out the many complex responsibilities of the role. Other staffing recommendations for improving infection control include:
- Ensuring that every nursing home has a dedicated infection preventionist responsible for developing and implementing IPC policies, surveillance and data collection, outbreak management, staff training and oversight of proper IPC procedures in the home.
- Directing facilities to provide comprehensive and regular IPC training to all staff. Training should include not only clinical staff, but also environmental services, housekeeping, dietary, activities and administrative roles, among others.
- Providing funding to support paid time for staff to go through comprehensive IPC training and requiring that nursing homes certify that the training is complete.
- Providing incentives for nursing homes to adequately compensate CNAs so that they are not forced to take on second and third jobs.

Building, designing, constructing, renovating and upgrading systems are other important areas for IPC. This recommendation includes funding for nursing homes to upgrade physical-plant systems and improve heating, ventilation and air conditioning. In addition, offering incentives to convert nursing homes to single-occupancy rooms would support IPC improvement efforts.
Responsive financial models and adequate funding and resources would promote and sustain effective IPC efforts. This recommendation includes:
- Offering funding and support to integrate robust infection surveillance systems into existing nursing home data collection processes.
- Collaborating with federal and state agencies to ensure that all nursing homes have access to an adequate supply of medical-grade personal protective equipment.
- Requiring greater transparency in ownership structures and business models, particularly in for-profit nursing homes.
- Liberating millions of dollars of civil monetary penalty (CMP) funds from bureaucratic complexity and specifically prioritizing these funds for IPC improvements.
The last area for IPC recommendations is related to survey and regulatory matters. For example, developing a pre-regulatory consultative support system, separate from survey agency oversight, would promote better nursing home accountability and compliance with the CMS Requirements of Participation. Other recommendations include:
- Amending the survey process so that it does not punish a nursing home for the desired behavior of gathering data and voluntarily reporting deficiencies; only for hiding or not reporting these.
- Establishing a Centers of Excellence in Infection Prevention and Control program to recognize those nursing homes with stellar IPC practices and outcomes.
To be sure, the COVID-19 pandemic did not cause the current crisis in nursing home IPC, but it most certainly revealed the systemic flaws in this key process, resulting in tragic and disproportionate levels of sickness and death among our vulnerable nursing home population. The Advancing Excellence Collaborative has developed important and urgent policy recommendations for CMS and other government agencies to implement to support nursing home residents and their families, along with nursing home staff, during the pandemic and beyond. This set of recommendations may serve as the foundation of a federal regulatory framework that addresses the root causes of long-standing IPC deficiencies in PALTC settings.
To learn about all the Advancing Excellence recommendations, look for the remaining articles in this series in McKnight’s Guest Columns.
Christopher E. Laxton, CAE, is immediate past chair of the Advancing Excellence in Long-Term Care Collaborative. He serves as Executive Director of AMDA – The Society for Post-Acute and Long-Term Care Medicine.
Patrick Luib, NP, serves on Advancing Excellence as a representative for the Gerontological Advanced Practice Nurses Association (GAPNA). He is the current chair of the Post-Acute and Long-Term Care Special Interest Group and a member of the Health Affairs Committee for GAPNA.
Theresa Schmidt, MA, is the 2021 Secretary of Advancing Excellence and has served on the board since 2014. In this role, she led the development of the open letter to the Biden Administration. She is a Vice President at Discern Health, part of Real Chemistry.
The Advancing Excellence in Long-Term Care Collaborative is a not-for-profit entity that creates a forum for organizations and individuals committed to the needs of long-term care residents and staff to discuss policies that affect these vulnerable populations.
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.







