
It’s surprising that the type and amount of post-acute care patients receive after discharge partly depends on which hospital provided their acute care.
Data show that hospitals in the same community use post-acute care services at very different rates, and across the country the use of inpatient rehabilitation facilities, skilled nursing facilities and home health services varies even more.
Although it is difficult to determine the proper rate of use of PAC services because needs differ across communities, the level of variability of use of PAC services points to opportunities to correct both overuse of inpatient facilities and potential underuse of home health services. Overuse of PAC services is a problem because it represents waste — costs and utilization that do not improve the health of the patient. Underuse of PAC services is also challenging because it can result in higher costs of care due to readmissions and potentially preventable expenses.
Fortunately, by using data to identify high-performing PAC facilities and home health agencies, creating preferred PAC partnerships using a value-based approach, and providing discharge management including data-driven choice of facilities and home health agencies, it is possible to improve the efficiency and effectiveness of PAC services.
How much does variability in use of PAC services affect costs?
An Institute of Medicine study found that variations in PAC spending were the single greatest driver of regional differences in Medicare spending when controlling for wages and local costs. Additionally, spending on PAC services doubled between 2001 and 2011, making it the fastest-growing part of the healthcare system.
Since that time, PAC spending has slowed a little, but in 2015, Medicare spent over $60 billion on PAC services.
If all of those dollars were being spent on effective, efficient care, that would be fine. But the level of variation, despite similar populations and the high growth in PAC utilization, suggests that some of the care is wasteful and not adding value.
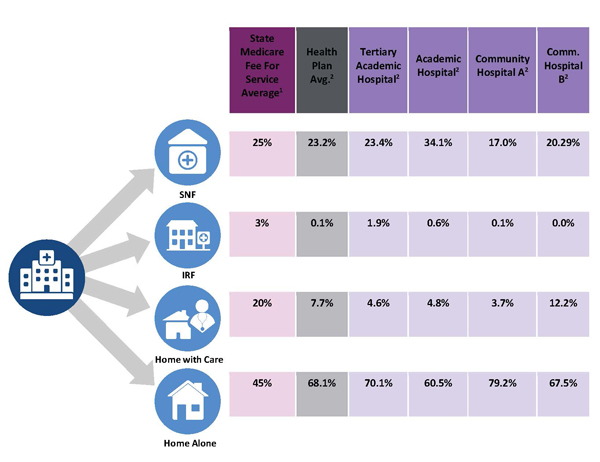
Figure 1 (below) shows a CareCentrix analysis of discharge patterns for several local hospitals, compared to the Medicare Advantage plan average and the state average for Medicare fee for service beneficiaries. Each column shows the percentage of discharged patients referred for PAC services for the state, health plan members, or for a specific hospital. Even though these hospitals are in the same community, there is significant variability and odds are that not all of it is driven by patient need.
Consider referrals to SNFs: For the state, 25% of discharged patients go to a SNF, for the health plan it is 23.2%, and for the hospitals it ranges from 17% to 34%. Admittedly, these hospitals serve different populations, but the academic hospital that sends over one-third of its patients to SNFs, sends more patients there than the tertiary academic hospital across the city, and double the rate of the suburban hospital 20 minutes away.
This variation reflects different discharge planning processes, clinicians with varying levels of comfort sending patients directly home after discharge, and probably overuse of SNF services.
The figure also shows that these hospitals are much less likely to refer patients for home health services compared to state averages. This may represent underspending, which is problematic since a recent study by Roy Xiao and colleagues at the Cleveland Clinic found that early referral and use of home health services actually reduced total costs of care for those hospitalized patients over the following year.
So what can be done to reduce variation in PAC service usage and improve use of home health services?
First, it is important to understand current practice patterns. Is there overutilization or underutilization of PAC facilities and home health use? In communities where there is high SNF usage, and lower home health usage, it may be possible to substitute home health services for SNF services and have more patients go directly home and not stay in the SNF.
Medicare Advantage plans often have these data and can share them with hospitals, SNFs, home health agencies and physician groups to encourage further evaluation of the causes of the current patterns of utilization and what can be done to improve it.
Another important opportunity is to create alignment between hospitals and the PAC facilities and home health agencies in their community. This allows for selection of higher performing facilities and home health agencies, and the selection and use of preferred PAC provider networks has been shown to reduce readmissions and improve care transitions by allowing hospitals to provide better communication and coordination of care, and the SNFs and home health agencies are better able to manage patients and reduce readmissions.
Financial alignment is also important. PAC facilities and home health agencies are still paid on a fee for service basis that offers greater revenue for performing more services. Moving them toward a more value-based approach that offers financial rewards for improved length of stay, reduced readmission rates, and better patient experience scores can help to offset lost fee for service revenue and engage them in quality improvement activities and staffing changes if needed.
The higher quality facilities and home health agencies tend to also attract greater volume over time, which offers more revenue and multiplies the rewards of providing higher quality care.
Transitions in care, from hospital to SNF, or hospital to home, or SNF to home, are potential clinical failure points, where errors can occur that increase the likelihood of readmission. Identifying patients at risk of readmission and using additional care management resources to smooth the transitions can improve care coordination and reduce readmissions.
Care managers working in hospitals and SNFs can collaborate with discharge planning teams to ensure coordination of services after discharge, and higher quality transitions of care. Transition coaches who work with patients discharged home can help patients create healthcare goals for their first 30 days after discharge and ensure that patients keep follow-up appointments, have the proper medications and are tied into any needed community resources.
Providing a data-driven approach to selecting the next level of care also can help. One recent study from Emily A. Gadbois and colleagues at Brown University found that the only information most patients and families considered when choosing a SNF was location and proximity to their home.
Medicare’s new policy of requiring hospitals to share information about SNF quality of care in addition to a list of names and locations of SNFs should help address this gap.
There is a significant opportunity to reduce wasteful healthcare expenditures by better managing PAC service use and the process used at hospitals to determine which patients get what kinds of services. Key steps in improving the efficiency of PAC service utilization include: providing data about PAC services to hospitals, patients and their families who are deciding what is needed after discharge; increasing use of home health services for patients who can benefit from additional support while transitioning home; working with selected PAC service providers to improve quality and patient experience; and providing care managers and transition coaches to ensure safe and successful discharge home.
[1] Benchmark data obtained from commercial vendor
[2] CareCentrix analysis of Health Plan claims data
Michael Cantor, MD, JD, is Chief Medical Officer at CareCentrix.



