
On a second day of hearings targeting the nursing home industry and its COVID-19 response, senators repeated calls for data and ownership transparency but also urged more federal and state support for home- and community-based services.
Sen. Elizabeth Warren (D-MA) called on Congress to require states to provide Medicaid coverage for such services as a way to keep patients out of nursing homes.
“The administration must strengthen nursing home standards in the wake of this pandemic, but the coronavirus has also highlighted the critical importance of providing care safely in home and communities,” she said during a virtual hearing of the Special Committee on Aging. “Here’s the problem: Millions of American can’t access HCBS services at home …. Congress must do more. It must do much more. We must make HCBS a mandatory benefit in Medicaid and expand Medicare to cover more at-home, long-term care services.”
Warren also said Congress should force private insurers to “commit some of their billions of dollars in profits to covering long-term care. Health care, including access to long-term care provided to people in their homes and communities, should be a right not a privilege.”
Much of the hearing, “COVID-19 One Year Later: Addressing Health Care Needs for At-Risk Americans,” focused on disparities in care during the pandemic. Speakers from acute-care settings and a senior advocacy group noted the virus had a disproportionate impact on the elderly, people with disabilities, minorities and rural Americans. That has been complicated by a vaccine campaign that has underserved many of those same groups, some of whom are hesitant to accept emergency-use vaccines, witnesses said.
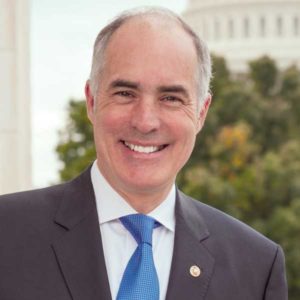
Committee Chairman Sen. Bob Casey (D-PA) authored provisions in the $1.9 trillion American Rescue Plan aimed at improving vaccine outreach and distribution; investing about $12.7 billion in home- and community-based services; and funding infection control training and strike teams to stop the spread of COVID-19 in nursing homes.
Comments also centered on access to care and the expansion of telehealth services, as well as programs that would strengthen the home care workforce.
Investments questioned
Anthony Jackson, senior vice president and chief operating officer of Roper Saint Francis Healthcare in Charleston, SC, is a former licensed nursing home administrator. He told senators nursing homes will need additional resources even if the government provides more support to home- and community-based networks.The current system, he said, puts regulations — such as requiring one registered nurse per shift — in conflict with the “pressures of reimbursement.”
“When you look at the viability of a nursing home, they started to move away from the responsibility for which they exist, which is to take care of patients from a long-term perspective,” he said. “They moved toward taking care of short-term types of disease which provides for quicker turnover and a better reimbursement.”
Thursday’s hearing also featured sternly worded reminders of a similar Senate Finance Committee hearing the day before, during which Warren excoriated Genesis HealthCare and for-profit operators and owners. She said she plans to launch an investigation into for-profit nursing homes, including those run by private equity firms.
Sen. Kirsten Gillibrand (D-NY) took up that mantle Thursday, citing a working paper by the National Bureau of Economic Research that found private equity in the industry had grown from $5 billion in 2000 to $100 billion in 2018.
“When private equity firms acquire nursing homes, patients start to die more often and taxpayers start paying more too,” she said. “We saw patient outcomes suffer and affordability become more difficult with the surprise billing situation that many experts claim was filed and exacerbated by private equity’s acquisition of hospitals and urgent care facilities. Could we expect similar outcomes with private equity in nursing homes?”



