Nursing home operators are grappling with audits targeting their use of schizophrenia diagnoses, a bounty of questions made clear during a national forum Thursday.
Providers took the Open Door call with Centers for Medicare & Medicaid Services officials as an opportunity to demand more information on the audit program, which began in late January. But leaders from two CMS divisions offered little in the way of additional details, except to report that the agency is examining whether it might adjust conditions that are linked to a measure tracking use of antipsychotic medications.
“We had a technical expert panel recently, and we are actively looking at these measures,” said Rebekah Natanov, quality measure lead with the Division of Chronic and Post-Acute Care.
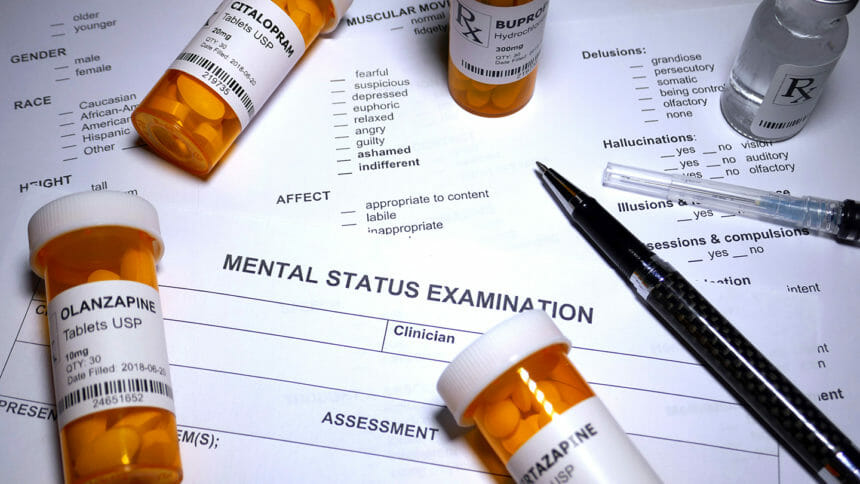
While nursing homes are discouraged from prescribing antipsychotic medications by a quality measure that corresponds with their use, prescriptions for patients diagnosed with schizophrenia, Tourette’s and Huntington’s disease are exempted from calculations.
Natanov’s comments reflect CMS’ intention to more carefully monitor the measure and, possibly, to make it more reflective of on-the-ground practices. The schizophrenia audits are designed, CMS said at launch, to determine if some facilities used that particular diagnosis to “mask” true rates of antipsychotic medication use.
If the agency finds a pattern of diagnosing not supported by proper assessment and documentation, it will drop quality measures for up to a year, a move that will affect a provider’s overall star rating.
Providers on the call Thursday expressed concern about how little detail they’d been provided on the audits, so far outlined only in a four-page memo. One provider asked what would constitute “proper documentation,” and an official from the Division of Nursing Homes said she could not answer the question.
Another caller asked whether a patient referred from a hospital to a nursing home with a schizophrenia diagnosis and related medications would be “sufficient enough” to meet audit requirements.
“If you have a diagnosis code, we’d expect you to do a comprehensive evaluation even if already diagnosed,” said Christine Teague.
Others asked CMS to look at hospital diagnosing patterns, with one nursing home participant saying, “That’s the point at which some of this starts.”
Teague said the agency was “aware that there are some challenges” and shared that with the agency’s hospital oversight branch.
Another concern raised: Audit results being appealed appear to be going to the same individual who conducted the first-round audit of a facility.
MDS and iQies changes also addressed
Also on Thursday’s call, CMS officials urged providers to continue tracking coming changes to MDS data sets, as well as a major change to the system used to submit such reports.
The current MDS system will transition to the Internet Quality Improvement and Evaluation System, or iQIES, portal effective April 17. Prior to that date, all facilities must have a designated security official, but a CMS official said that only 76% have completed the required steps.
After a three-day transition period during which providers will have no access to MDS systems or reports, the new system will be up and running ahead of implementation of the latest MDS data set and manual.
Officials said they will post finalized data sets and a draft RAI manual in April, followed by final MDS data specifications in May and a finalized RAI manual in August. The new MDS requirements, including elimination of Section G, is scheduled for Oct. 1.
CMS will host a series of virtual workshops on the changes and give providers opportunities to practice coding between May and July.



