
Skilled nursing patients received about 13% fewer therapy minutes after the onset of the Patient-Driven Payment Model in October 2019 but that did not hurt outcomes or rehospitalization rates, researchers have found.
That means the Medicare payment system was working as intended during the six-month period before and just after the pandemic was declared in March 2020, investigators told McKnight’s Long-Term Care News.
Some of the same researchers determined earlier that therapy staff was reduced about 5% upon conversion from the therapy-based Research Utilization Groups (RUGs). This study, however, is the first to look at whether therapy declines had any significant impact on care outcomes. It was released Friday by JAMA Health Forum.
“We didn’t see any changes in ADL scores at discharge,” explained lead researcher Momotazur Rahman, P.h.D., of the Department of Health Services, Policy & Practice, at Brown University’s School of Public Health. “We tried it many ways to see if we were doing anything wrong, and the result was no change. That would imply that there was too much therapy provided before.”
The researchers compared MDS and beneficiary summary records of more than 201,000 fee-for-service Medicare patients, about one-fourth admitted post-PDPM. They primarily focused on hip-fracture patients but also replicated results in the overall study sample. Data from admission day, the 5-day scheduled assessment and discharge were common assessment points between the payment systems.
Total net therapy averaged about 12 minutes (13%) lower once PDPM kicked in. Therapy utilization was measured by combining patients’ total number of physical, occupational and speech therapy minutes.
Meanwhile, hospital readmissions rose a statistically insignificant 0.31 percentage points; expected SNF length of stay beyond 40 days fell 2.7 percentage points; and activities of daily living scores at discharge increased 0.04 points.
“We’re finding no significant changes — no harm so that they’re being rehospitalized more or have to stay in the SNF for longer periods,” noted researcher Brian McGarry, Ph.D., of the University of Rochester’s Department of Medicine, a non-practicing physical therapist. “In general, it looks like PDPM was working largely as intended in the intermediate term. Then COVID hit, so the effects of PDPM long-term will remain a mystery for a while.”
No fond farewell
Study results, however, left no mystery about the RUGs system, he added.
“If therapy was being dispensed strictly on need factors, you would expect normal distribution patterns, that is a bell curve based on clinical presentation and therapists tailoring amounts of therapy to individual needs,” McGarry explained. “Clearly, under RUGs that was not the case. There were targets therapists were steering to hit, to maximize reimbursements, and they were very successful in doing that.
“PDPM overnight took that distribution and returned it to what we consider normal distribution,” he added. “Now therapy minutes are distributed clinically.”
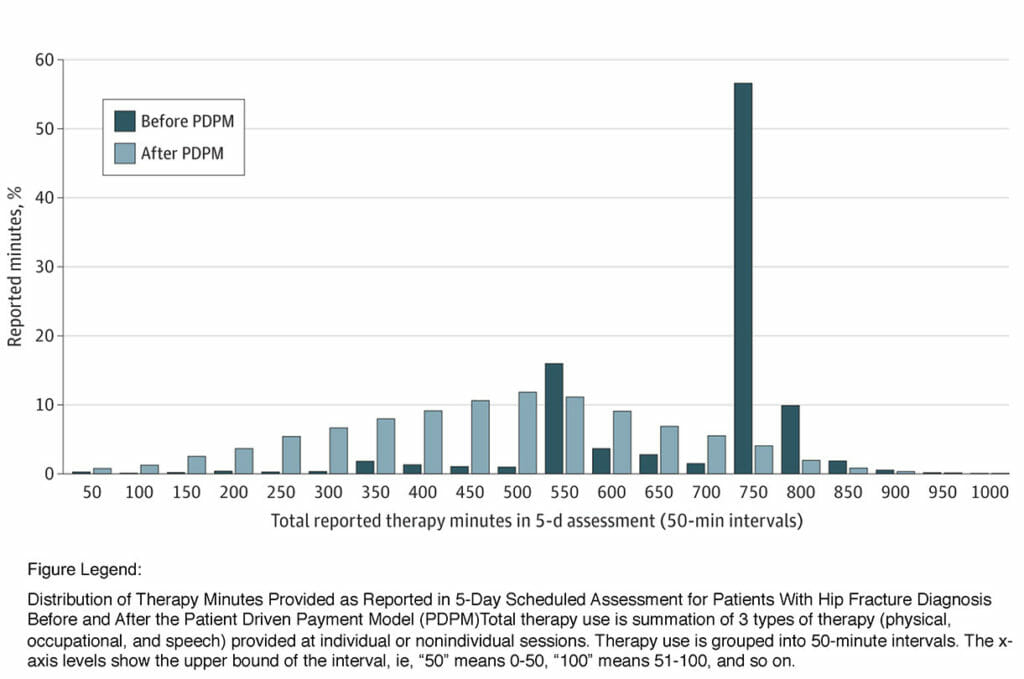
Researchers found that under the RUGs system, utilization spiked in the 501- to 550-minute and 701- to 750-minute intervals. That was “consistent with the 500-minute threshold for the high therapy group and the 720-minute threshold for the ultrahigh therapy group,” respectively, they noted. More than 55% of patients received “just enough” therapy to be in the Ultra High category, they added.
Under PDPM, the bell curve shows usage peaks in the 451-to-500-minute interval.
The researchers said PDPM appears to have brought positive effects for both therapists and provider organizations.
“PDPM is actually giving a little more autonomy to therapists to tailor their therapy recommendations based on needs, as opposed to some arbitrary benchmark,” McGarry noted. He added that therapy groups, among others, will rightfully want to remain vigilant that pressures to hold down costs don’t result in insufficient treatment levels that hurt outcomes.
Meanwhile, the broader criteria for awarding Medicare reimbursements is helping most providers, according to study leader Rahman.
“That has increased reimbursement for newly admitted patients, relative to the budget-neutral case [that PDPM was founded on],” he said. “At the same time, we know patients are receiving fewer therapy minutes, so the cost of providing post-acute care has declined.”
Other members of the research team included Elizabeth M. White, APRN, Ph.D., Christopher Santostefano, BSN, RN, Peter Shewmaker, ScM, and Linda Resnik, PT, Ph.D., all of whom share the Brown University affiliation with Rahman; and David C. Grabowski, Ph.D., of the Department of Health Care Policy at Harvard Medical School.
Findings were published as an open access article at JAMA Health Forum.




