
Supplemental benefits designed to address seniors’ health and well-being have long targeted community-dwelling beneficiaries. They have grown from simple dental and vision add-ons to a wide swath of extras ranging from meals to pest control.
But residents of skilled nursing facilities, where most medical support is already covered, have largely missed out on such added benefits.
Recently, however, a growing number of Medicare Advantage plans serving nursing home residents are picking up the cost of added services, such as resident companionship, music therapy and transportation. Under updated regulations these services can be covered because they help address isolation and other psychosocial needs.
Such benefits can be a boon to skilled nursing providers who partner with Institutional Special Needs Plans. The plans provide additional caregivers and other supplemental support to improve quality of care, and connected facilities can earn a reputational boost at no additional cost to them or their residents.
ATI Advisory said it has seen an increase in I-SNPs’ supplemental offerings, though in limited categories.
“While we have seen some I-SNPs use new supplemental benefit authorities, we haven’t seen them use it as the same rate as the general MA population or as much as C-SNPs or D-SNPs,” said Tyler Overstreet Cromer, principal and head of ATI’s Medicare Innovation Practice, referring to plans that target chronically ill people or those with disabilities.
But as more plans begin to explore their options for nursing home residents, Cromer sees plenty of opportunity for creative solutions.
“There’s a really big runway here,” she said. “I would really encourage plans to think about what they can do with these authorities and to talk to their facility partners about what would be meaningful to them and their residents and design benefit packages that help fill those needs.”
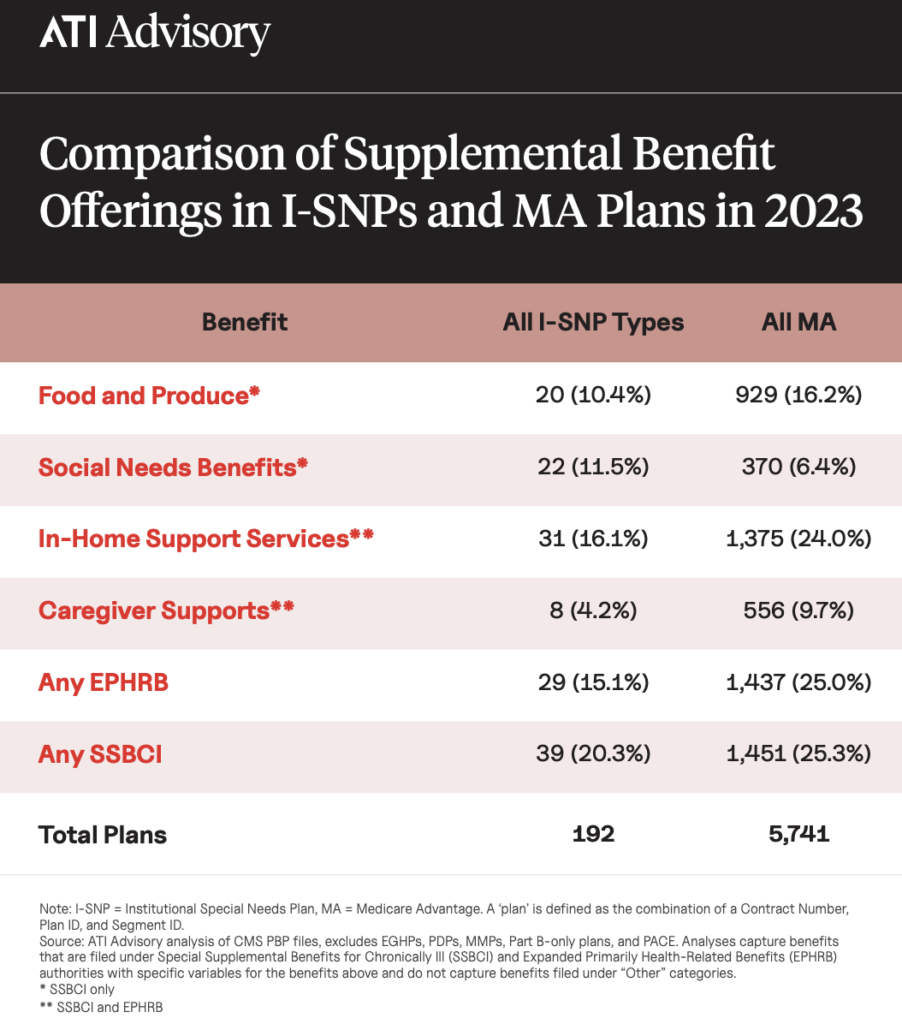
ATI mines official MA plan data from the Centers for Medicare & Medicaid Services and conducts interviews with plans to gather its insights. For 2023, Cromer’s team found the only area where a larger share of I-SNPs are offering supplements than the broader MA market is in the social needs benefit category, at 11.5% of plans. Overall, just 6.4% of other MA plans offer similar services.
New services offered
Longevity Health has expanded its offerings from basic hearing, vision and dental supplements to include such diverse options as specialized music therapy and companionship services for patients with dementia or behavioral health diagnoses.
The firm’s clinical approach already adds nurse practitioners and other advanced clinicians into skilled nursing facilities to supplement staff. But the companionship model has had renewed interest — and success — since facilities reopened doors to visitors after Covid closures.
“Historically, what we saw happen quite a bit is if you have that member who has the behavior change and there’s no one there with them to de-escalate and listen to them, what happens?” asked Marc Hudak, the company’s chief growth officer and IPA business lead. “They get admitted to the hospital. That’s not a good outcome for anyone. They just need someone to spend time with them while an alternative treatment plan is being developed.”
Hudak said companionship programs have reduced overuse of hospitalization, leading SNF partners to ask that Longevity invest more in the program to make companions available for more hours.
Longevity also is expanding use of a karaoke-like music therapy program, which has been clinically developed to elevate mood, improve cognitive function, reduce stress and anxiety and promote reminiscence. Beneficiaries also can shop from a health products catalog four times a year, spending $210 on products such as blankets, magnifying glasses and more.
AllyAlign Health currently serves over 7,500 Medicare beneficiaries across 16 states. President Jeremy Dressen said the company works closely with its nursing home and assisted living partners to design benefits and adjust offerings “to remain competitive and continue to meet the unique needs in a market or facility.”
Most of AllyAlign’s I-SNP plans provide comprehensive dental (including mobile dentistry), vision coverage, podiatry visits, non-emergency transportation and a quarterly allowance to purchase over-the-counter medications and other flexible-spending eligible items, such as personal hygiene products.
Marketplace wave
Supplemental benefits began to explode in 2019, when federal regulators expanded the definition of “primarily health related” benefits to include items such as in-home and personal care, adult day care and caregiver support.
Those MA supplemental services were well-suited to seniors who needed help at home, and they also could have helped some recipients stay in their own homes for longer — a cost-reducing goal of many Medicare Advantage plans.
Beginning in 2020, plans could also offer a new line of benefits for the chronically ill, and that was followed in short order by the inclusion of benefits addressing social determinants of health. The latest set of interventions can address food insecurity, home safety modifications, transportation needs and more.
Plans can expand their offerings annually by submitting to CMS bid details such as external expertise on value and use and cost estimates.
Moving forward, Cromer and ATI Director Bill Winfrey said they expect to see use of companionship — viewed as meaningful by residents, families and facilities — continue to grow.
Winfrey said he can envision plans beginning to allow beneficiaries to select their own paid companions, as well as plans that offer caregiver assistance to loved ones that help care for residents in their nursing homes.
Transportation to medical appointments and non-medical activities also could be a key tool to keep residents connected to the outside world and improve their quality of life, Cromer said.
Hudak said selecting new benefits is a balancing act between building interest and enrollment in the plans and finding investments that help skilled nursing partners improve health and well-being in measurable ways.
“There are a lot of constituents,” he said. “These flexibilities that CMS is allowing are understanding that there is a broader set of health benefits to be considered. It is an exciting time.”




