The Centers for Medicare & Medicaid Services will establish minimum staffing requirements as part of a broad plan to “crack down on unsafe nursing homes,” the White House announced on Monday.
The agency said it plans to conduct a new study to determine the level and type of staffing needed to ensure safe and quality care and will issue proposed rules within one year.
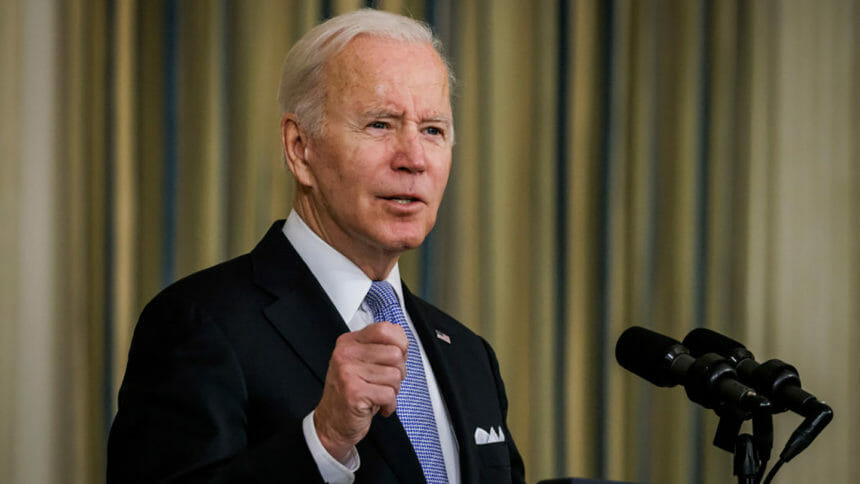
The reform measure is part of four new initiatives to ensure that residents get the quality care they need, according to the White House. President Joe Biden plans to raise the initiatives, which are sure to chafe nursing home operators, during his State of the Union address Tuesday evening.
Biden also will call on Congress to supply almost $500 million to increase CMS’s survey budget by nearly 25%, an administration statement said.
The new initiatives also include plans to reduce resident room crowding, with CMS planning to explore ways to accelerate phasing out rooms with three or more residents and to promote single-occupancy rooms.
The agency also intends to update the Skilled Nursing Facility Value-Based Purchasing Program by proposing new payment changes based on staffing adequacy and the resident experience, as well as how well facilities retain staff.
Lastly, the agency will launch a new effort to identify what it calls problematic diagnoses and refocus efforts to continue to bring down the inappropriate use of antipsychotic medications.
The Biden administration also pledged to ramp up its accountability and oversight of nursing homes and called on Congress to raise the dollar limit on per-instance financial penalties levied on poor-performing facilities from $21,000 to $1,000,000.
Failure ‘widespread’
The administration delivered a general broadside to nursing home operators while announcing the new plans.
“In the past two years, more than 200,000 residents and staff in nursing homes have died from COVID-19 — nearly a quarter of all COVID-19 deaths in the United States,” the White House statement stated. “Despite the tens of billions of federal taxpayer dollars flowing to nursing homes each year, too many continue to provide poor, sub-standard care that leads to avoidable resident harm. In fact, failure to comply with Federal guidelines at nursing homes is widespread.”
It cited a Government Accountability Office report that found that, from 2013 to 2017, 82% of all inspected nursing homes had an infection prevention and control deficiency, “including a lack of regular handwashing,” that was identified through Medicare and Medicaid surveys.
“Without decisive action now, these unacceptable conditions may get worse,” the administration said.
Officials said that establishing minimum staffing levels will ensure that residents will be provided “safe, quality care, and that workers have the support they need.”
“Nursing homes will be held accountable if they fail to meet this standard,” they noted.
The consumer-facing Care Compare website will “prominently” display whether a facility is meeting future minimum staffing requirements. The agency also will “ensure that ratings more closely reflect data that is verifiable, rather than self-reported, and will hold nursing homes accountable for providing inaccurate information. “
In addition, President Biden will ask Congress to expand CMS’ powers so it can validate data and take enforcement action against facilities that submit incorrect information.
“CMS intends to propose new payment changes based on staffing adequacy, the resident experience, as well as how well facilities retain staff,” officials added in the White House statement.
Private equity slammed
The administration announcement took especially harsh aim at private equity’s ownership of nursing homes.
“Private equity firms have been buying up struggling nursing homes, and research shows that private equity-owned nursing homes tend to have significantly worse outcomes for residents,” a fact sheet provided by the White House said.
It noted that private equity firms’ investment in nursing homes “has ballooned” from $5 billion in 2000 to more than $100 billion in 2018, with about 5% of all nursing homes now owned by private equity firms.
It explained a recent study found that residents in nursing homes bought by private equity were 11.1% more likely to have a preventable emergency department visit and 8.7% more likely to experience a preventable hospitalization, when compared to residents of for-profit nursing homes not associated with private equity.
Another examination over 17 years , a working paper, examined 18,000 nursing facilities and found that private equity ownership increased “excess” resident mortality by 10%, increased prescription of antipsychotic drugs for residents by 50%, decreased hours of frontline nursing staffing by 3%, and increased taxpayer spending per resident by 11%.
“That suggests an additional 20,150 lives lost as a result of private equity ownership,” the administration said. Another study found that private equity-backed nursing homes’ COVID-19 infection and death rates were 30% and 40% above statewide averages, respectively.
“Too often, the private equity model has put profits before people — a particularly dangerous model when it comes to the health and safety of vulnerable seniors and people with disabilities,” the White House statement said. “Recent research has found that resident outcomes are significantly worse at private equity-owned nursing homes.”
CMS targets SFF facilities, corporate owners
The administration also intends to come down harder on consistently poor performing facilities.
The Special Focus Facility program will be “overhauled to more quickly improve care … including changes that will make its requirements tougher and more impactful.”
“Facilities that fail to improve will face increasingly larger enforcement actions, including termination from participation in Medicare and Medicaid, when appropriate,” the administration said.
CMS also will expand how often it will penalize poor-performing facilities based on desk reviews of data submissions, which will be performed in addition to on-site inspections.
It said that beyond previously reversing President Trump’s move to levy one-time fines on “bad actor nursing homes,” CMS will now explore making such per-day penalties the default penalty for non-compliance.
The administration also wants Congress to give CMS added authority to “require minimum corporate competency” so that individuals or entities can be barred from obtaining a Medicare or Medicaid provider agreement for a nursing home if they have had compliance problems, past or present.
President Biden also will ask Congress to allow CMS to levy penalties and enforcement actions on owners or operators, even after a poor-performing building is closed.
In addition, CMS will increase pressure on corporate owners and operators by creating a new database that will track and identify owners and operators across states “to highlight previous problems with promoting resident health and safety.”
The agency also plans to collect and publicly report “more robust” corporate ownership and operating data, according to the White House briefing statement.
Senior administration officials earlier Monday said the reform measures are part of new actions that the Biden-Harris administration is taking this year to tackle some of the most pressing competition and consumer protection problems across our economy. Included would be “new steps to protect seniors and other nursing home residents by cracking down on unsafe nursing homes.”




