The Centers for Medicare & Medicaid Services has been monitoring and conducting “very comprehensive data analysis” to identify any trends or changes in provider behavior, payments and beneficiary care quality since implementing the Patient Driven Payment Model, agency leaders said Thursday.
“This is something that we talked a lot about prior to PDPM being implemented, that we would be looking at a wide variety of metrics, because looking at these metrics, understanding what impact this new payment model has had on new beneficiaries and the impact it’s had on facilities and just trying to piece all that together is very interesting, to be frank,” said John Kane, technical advisor and SNF payment team lead for CMS, at a Thursday session of the American Association of Post-Acute Care Nursing 2021 Conference.
He added, “But also it’s extremely important in trying to understand where we need to go from here.”
His comments come as the agency looks at amending PDPM’s parity adjustment after SNF spending under the model unintentionally increased by $1.7 billion, or 5%. The agency is also seeking provider input on a potential methodology for recalibration.
To understand PDPM’s impact, the agency uses data collected both prior to and after its implementation in Oct. 2019. Kane explained that CMS has been able to clearly identify which changes in SNF data are driven by PDPM, as well as those influenced by the COVID-19 public health emergency.
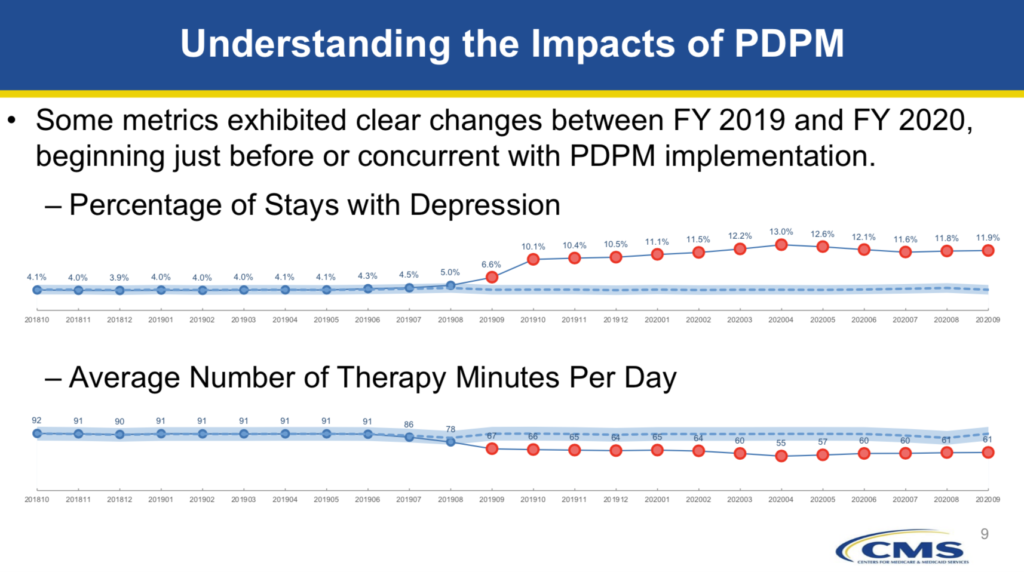
For example, Kane noted that SNF quality metrics that experienced no change between fiscal years 2019 and 2020 included percentage of stays with oxygen therapy and percentage of stays with dialysis. But the percentage of stays with depression (increase) and the average number of therapy minutes per day (decrease) exhibited clear changes during the timeframe just before or concurrent with PDPM’s implementation.
Metrics that changed with the onset of COVID-19 include the percentage of stays with infection isolation and percentage of long-term care nursing home stays in SNFs, which both increased.
Kane also noted there are cases where SNF data changed under PDPM and then changed again with COVID-19. In some instances, CMS has combined multiple metrics to understand the payment model’s overall impact.
“These are the kinds of things that we look at and do help to inform any sort of future policy development,” Kane said. “This is by no means to represent that we are fully done with our analysis of everything in relation to PDPM … But it’s also to indicate that we have done analyses, and that we do have a variety of analytics and metrics that we have been able to look at that have led us to questions — questions that we want to put before stakeholders, such as yourselves, so that we can get the important feedback that we need.”
Comments on the SNF Prospective Payment System for fiscal year 2022 are being accepted through June 7, 2021.





