
The Department of Health and Human Services should look for ways to provide broader patient access to new and future Alzheimer’s treatments, two congressmen say.
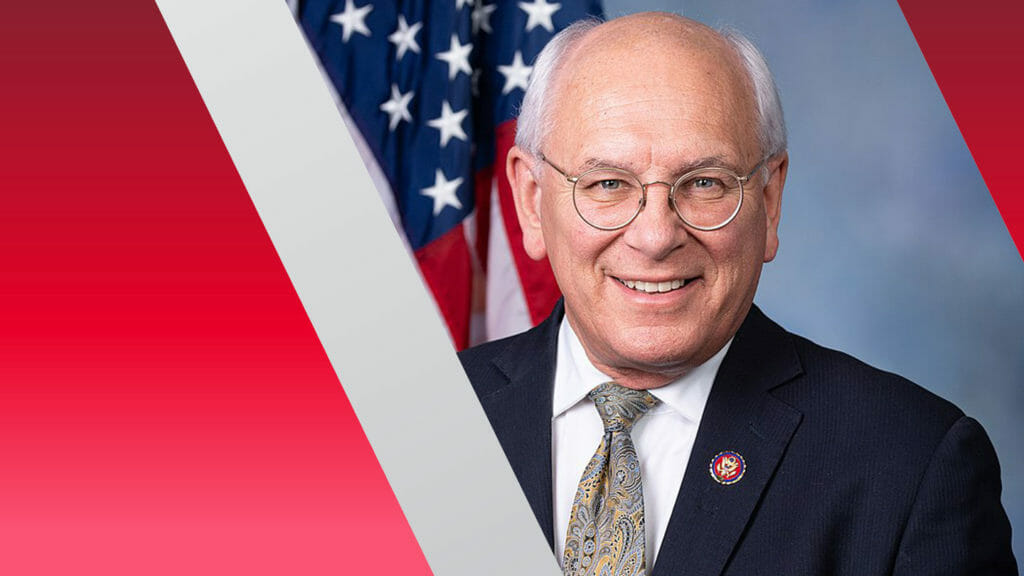
In a letter sent to HHS Secretary Xavier Becerra on Monday, Paul Tonko (D-NY) and Darin LaHood (R-IL) expressed concern that the agency’s proposed National Coverage Determination for the dementia drug Aduhelm will severely limit the number of patients who can benefit from it.
Aduhelm is a monoclonal antibody that targets and may reduce Alzheimer’s plaques in the brain. The Food and Drug Administration approved the drug — the first of its kind — despite concerns about its efficacy, safety, accessibility and affordability. In an unusual move, the Centers for Medicare & Medicaid Services in early January proposed that it cover the cost of Aduhelm treatment only for highly qualified participants in approved clinical trials.
In their letter, Tonko and LaHood said the proposal will impose a “certain and lengthy delay” in access to these treatments while new clinical trials are designed, approved and established. They asked HHS, which oversees CMS, to justify its decision to limit coverage in this way
The lawmakers also questioned the agency’s decision to preemptively impose the same coverage limits on similar drugs before they are FDA-approved, and asked what assistance would be available to researchers to help them recruit patients from minority communities, which historically have low participation in clinical trials.
Long-term care clinicians initially spoke up against the use of Aduhelm in residents, citing safety and administration concerns. But patient advocates have pushed for wide availability to those who wish to try it.
CMS has said that its coverage proposal is appropriate for the Medicare population. A final decision is expected in April.



