For the first time, the Centers of Disease Control and Prevention has identified U.S. nursing home residents and hospital patients with candida auris yeast infections that resist all first-line antifungal treatments, the agency reported Friday.
Among 101 infected nursing home residents identified between January and April 2021 in Washington D.C., three were resistant to all three drug classes known to combat the invasive yeast: azoles (fluconazole), amphotericin B, and echinocandins. Echinocandins are considered a critical defense against these infections, the CDC stated in its Morbidity and Mortality Weekly Report.
At the same time, agency investigators found two Candida auris infections in two Texas hospital system facilities that did not respond to any of the three antifungal drugs, and five patients who were resistant to two of the drugs: echinocandins and fluconazole.
These new cases of infections resistant to all lines of defense are concerning — especially those that defy treatment with echinocandins, CDC said. In the United States, candida auris usually responds to echinocandin, failing to do so in only about 1% of cases. In contrast, it resists the other two topline drugs much more frequently: azoles 85% of the time and amphotericin B 33% of the time, the agency reported.
“Echinocandin resistance is a concerning clinical and public health threat, particularly when coupled with resistance to azole and amphotericin B (pan-resistance),” agency investigators wrote in their report.
Nursing home residents at high risk
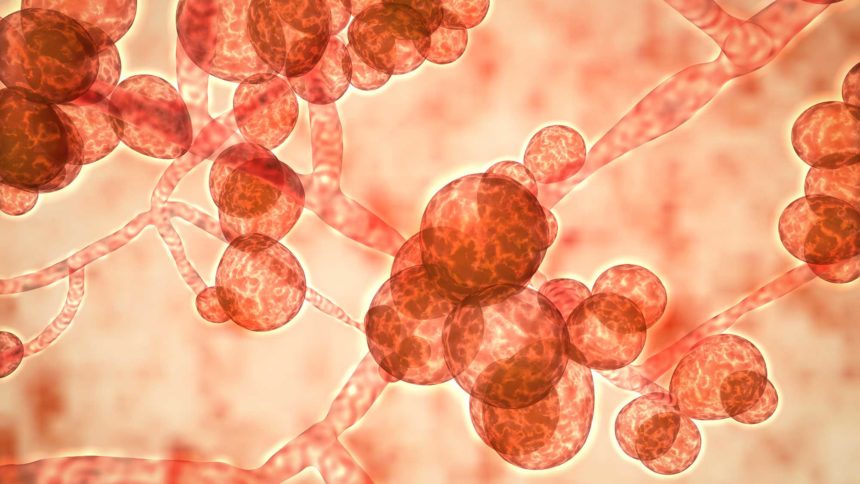
Candida auris is highly contagious, and has begun spreading rapidly in the United States, CDC said. Fully 5% to 10% of patients colonized with Candida auris are likely to develop invasive infections, with the infection accounting for up to 60% of the deaths in these cases, the CDC states.
At greatest risk of infection are those with tubes and lines going into the body, the American Council on Science and Health has reported. The fungus can grow on intravenous lines and ventilators. In fact, most cases have occurred in nursing homes that care for ventilated residents and in long-term acute care hospitals, according to the Illinois Department of Public Health. (Chicago is the site of a large number of U.S. infections.)
The CDC has identified more than 2,000 Candida auris cases in Americans over the past eight years, according to the New York Times. Most cases have been found in New York, New Jersey, Illinois and California, the news outlet reported.
Infection prevention and control
Candida auris is difficult to eradicate. It can colonize on the skin and spread from there — possibly when patients naturally shed skin cells, according to a key study in a Chicago skilled nursing facility. It has been found on every surface of infected patients’ rooms, and can remain in rooms even after thorough cleaning.
The CDC has posted infection control recommendations for prevention of Candida auris transmission in healthcare settings. These include:
- Adherence to hand hygiene,
- Appropriate use of transmission-based precautions based on setting,
- Cleaning and disinfecting the patient care environment (daily and terminal cleaning) and reusable equipment with recommended products,
- Inter-facility communication about patients’ Candida auris status when patients are transferred to another healthcare facility,
- Screening contacts of newly identified case patients to identify Candida auris colonization, and
- Laboratory surveillance of clinical specimens to detect additional cases.
The detailed recommendations are available here, including information about practices to reduce transmission in shared rooms and the most effective infection control products.
Related story: Deadly fungus colonizing SNFs sheds with patients’ skin, explaining widespread contamination



