The head of the Centers for Disease Control and Prevention stressed the need for repeated testing among staff members to stop the spread of COVID-19 in nursing homes.
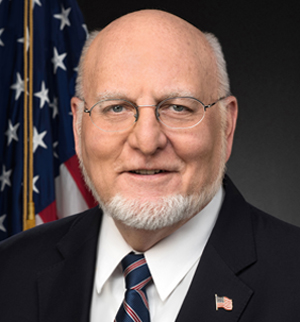
“Our experience continues to show that rapid and wide-scale testing in response in a setting of the nursing home to a new case is the best way to limit the transmission,” CDC Director Robert Redfield, M.D., said during a call with nursing home stakeholders Tuesday evening.
“There can be a substantial increase in the number of individuals that actually become infected based on delays of even several days. It’s critically important in these settings to have follow-up, repeated rounds of testing until no new cases are identified,” he added.
The Centers for Medicare & Medicaid Services in late August announced new federal regulations that mandates nursing homes test all staff members for COVID-19. The changes are part of an overall effort to identify asymptomatic people in facilities who could inadvertently spread the virus throughout buildings, the agency explained.
“We would like to underscore how important it is to conduct comprehensive testing as part of outbreak investigations. In the setting of long-term care facilities, we actually define an outbreak now as any [single] new case in a nursing home in a resident or a staff person,” Redfield explained.
Fines for non-compliance start at $400 per day and can reach up to $8,000, and possible termination from the Medicare and Medicaid programs and denial of payment for new admissions.
Good-effort required
Federal officials also announced that laboratories conducting COVID-19 testing, including nursing homes using point-of-care testing devices, are now being required to report test results daily to the Department of Health and Human Services. Those that don’t comply could be subject to fines of up to $1,000 a day for the first day, and $500 for each subsequent day.
CMS staff on Tuesday also stressed that providers must make “every reasonable attempt” to comply with the federal regulations and document the attempts they do make.
“When we come out, surveyors are going to look to see what have you done to comply with this regulation or take into consideration those things that you have documented,” said Jean Moody-Williams, deputy director of the Center for Clinical Standards and Quality.
“There are civil monetary penalties that are associated with this, so again we ask that we will work with you and that you document the challenges that you might be experiencing,” she added.
Shari Ling, M.D., CMS’ deputy chief medical officer, added that the agency is “committed to working with the CDC to ensure a seamless reporting vehicle for nursing homes so that they can report the point-of-care antigen results. It may be through a vehicle that you’re accustomed to reporting, such as the National Healthcare Safety Network.”





